NEET Biology Notes For Chemical Coordination And Integration Endocrine System
The branch of biology that deals with the study of the endocrine system and its physiology is known as endocrinology. Thomas Addison is known as the father of endocrinology.
Glands of Body
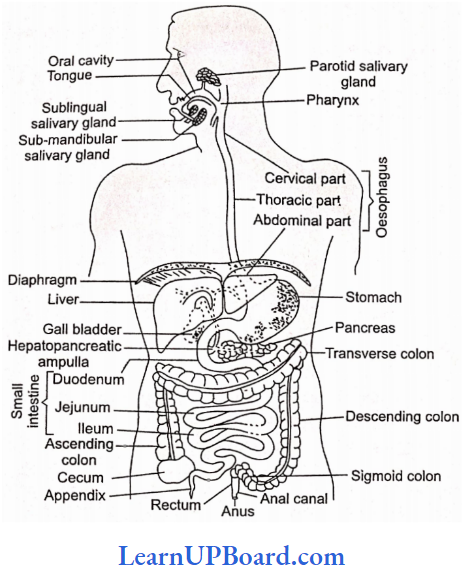
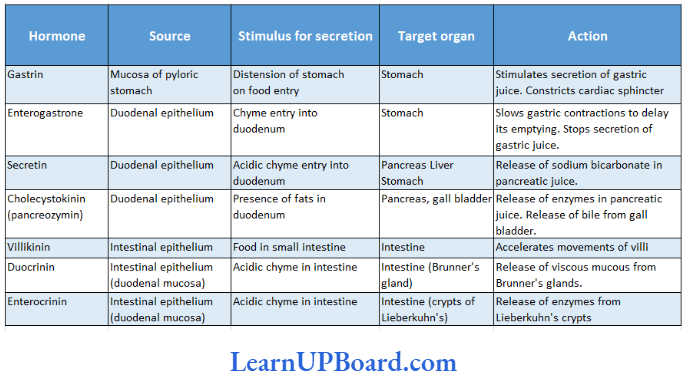
A cell, a tissue, or an organ that secretes certain useful chemical compounds is called a gland. Animals have three types of glands:
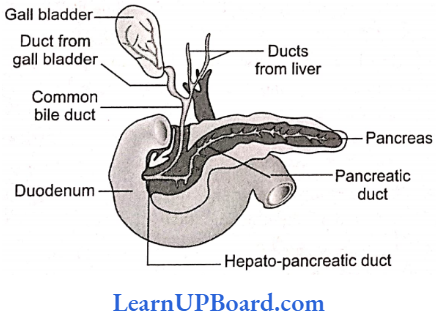
- Exocrine gland (Gr., ex = out + krinein – to secrete): These glands have ducts for discharging their secretions. Therefore, they are called duct glands. For example, the liver, sweat glands, sebaceous glands, gastric glands, and some intestinal glands.
- Endocrine glands (Gr., endo – within + kinetin = to secrete): These glands lack ducts and pass secretions into the surrounding blood directly. Therefore, they are called ductless glands. For example, thyroid, parathyroid, adrenal, pituitary, pineal body, and thymus.
- Heterocrine glands: These glands consist of both exocrine and endocrine tissues. The exocrine tissues discharge their secretion by a duct and the endocrine tissues discharge their secretion into the blood. Pancreas and gonads are heterocrine glands. These are also called mixed glands.
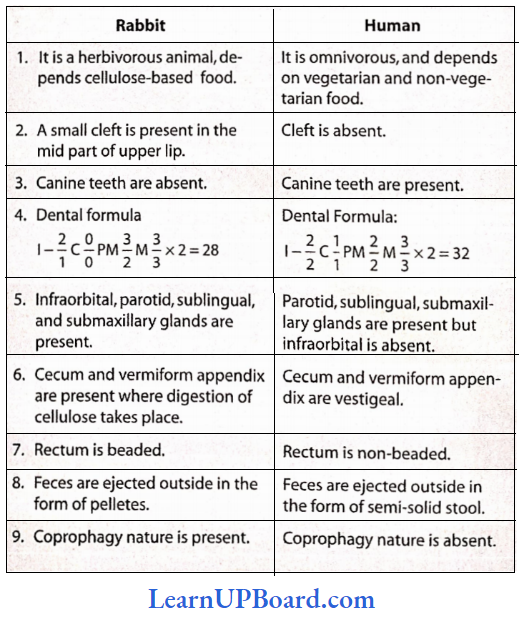
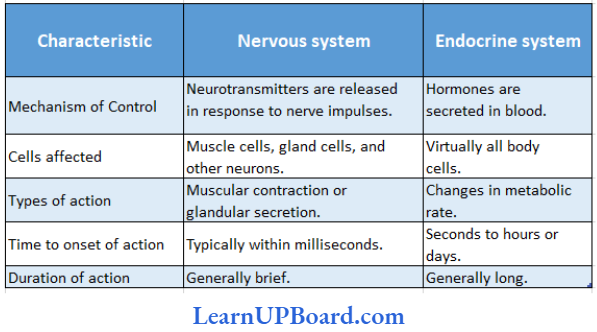
Coordination in the body of almost all the higher vertebrates is controlled by two systems: the nervous system and the endocrine system. The nervous system and endocrine system are called an integrative system of the body. The nervous system carries information in the form of impulses to different parts of the body. High-speed services are offered by this system, whereas the work of coordination by the endocrine system is slower due to the secretion of some chemical substances. Substances secreted by these glands are known as hormones. The meaning of the term “hormone” in Greek is to excite. Basic differences between nervous and endocrine coordination.
” chemical coordination and integration bank of biology”
Differences Between Nervous And Endocrine Coordination:
NEET Biology Notes For Chemical Coordination And Integration Hormone
The term “hormone” was coined by Starling. Hormones are also called primary messengers or chemical messengers.
- The first discovered hormone is secretin. It was discovered by Bayliss and Starling in 1902.
- Source and chemical nature: Hormones are chemical messengers that are secreted by one part of the body and are poured directly into the bloodstream, and they reach their target place with the help of blood. A small amount of hormone affects some specific cells or the physiology of the cells of an organ according to atmospheric conditions.
Read and Learn More NEET Biology Notes
Properties Of Hormones
The hormones have the following properties:
- They have low molecular weight.
- They are soluble in water and blood.
- They have no cumulative effect.
- They can act in low concentration.
- They are non-antigenic.
- They are organic catalysts.
Kinds Of Hormones
Based on their influence on physiological activities and control, the hormones may be divided into the following five categories.
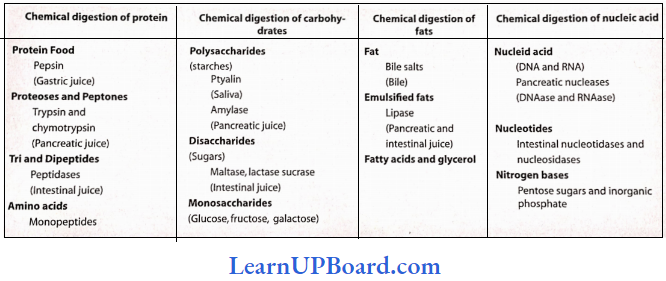
- Hormones concerned with metabolism, e.g., insulin, etc.
- Hormones for growth and development, e.g., somatotropin, etc.
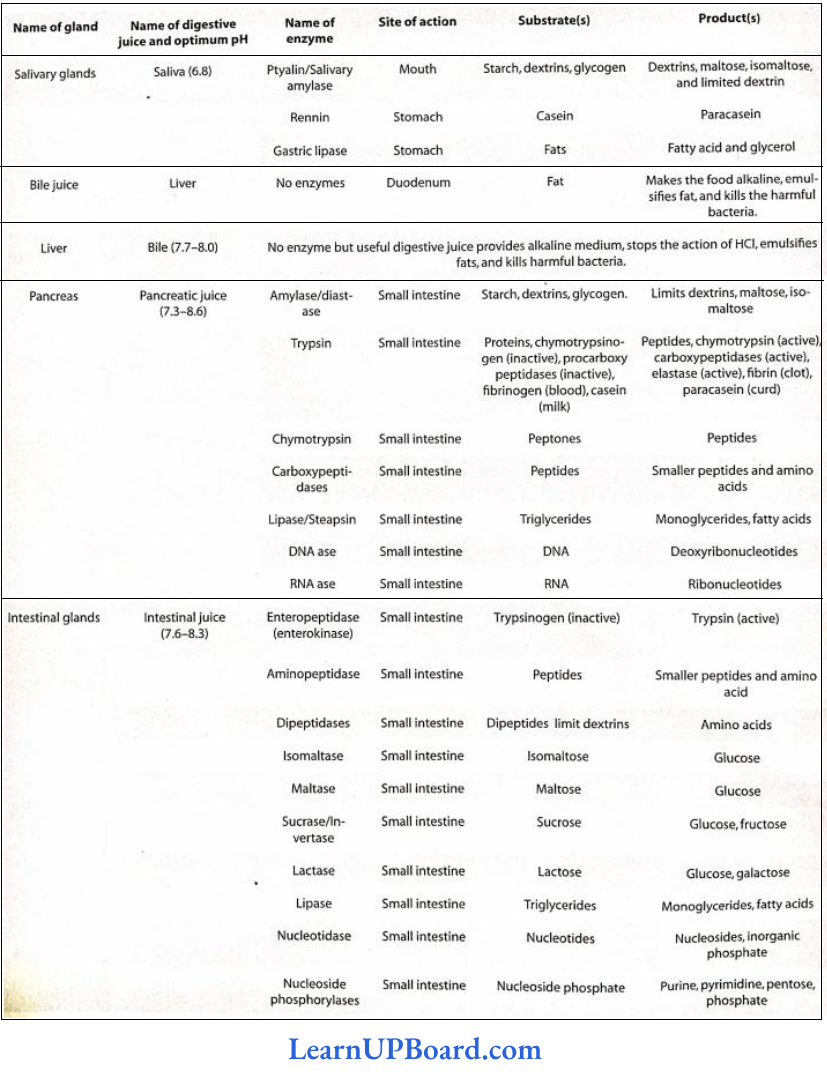
- Hormones of digestion, e.g., gastrin, secretin, etc.
- Hormones for reproduction, e.g., gonadotropin and sex hormones.
- Hormones that control other endocrine glands, e.g., thyrotropin, etc.
NEET Biology Notes For Chemical Coordination And Integration Hormone Points To Remember
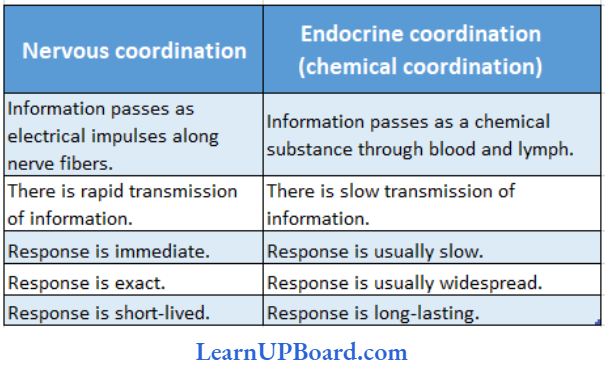
Differences Between Nervous System And Endocrine System
Biochemical Classification of Hormones
All hormones, depending on their chemical structure, may be classified under the following categories:
- Phenolic hormones: These are derived from an amino acid, tyrosine, e.g., thyroxine, adrenaline, nor-adrenaline, etc.
- Proteinaceous or polypeptide hormones: Examples are oxytocin, vasopressin, parathormone, prolactin, somatotropin, insulin, glucagon, secretin, relaxin, etc.
- Glycoproteinaceous hormones: Examples are thyrotropin, follicle-stimulating hormone, luteinizing hormone, etc.
- Steroid hormones: Pass directly through the plasma membrane because of lipid affinity and bind to receptors in the cytoplasm which in turn act on DNA. Examples are estrogen, aldosterone, cortisol, estradiol, progesterone, testosterone, and cortisone.
- Radioimmunoassay: Radioimmunoassay (RIA) is a technique to measure hormones, their precursors, and their metabolic end products quantitatively in a living body.
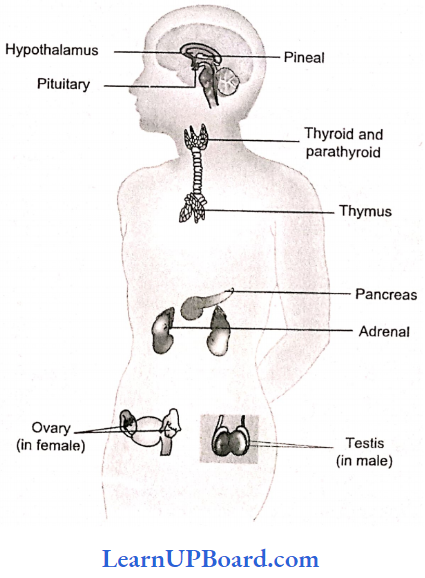
NEET Biology Notes For Chemical Coordination And Integration Types Of Endocrine Glands In Human
In man, the following major endocrine glands are present:
- Pituitary gland or hypophysis
- Thyroid gland
- Parathyroid gland
- Adrenal gland
- Islets of Langerhans in the pancreas
- Gastrointestinal lining
- Pineal gland
- Thymus gland
- Gonads
- Placenta
” chemical coordination and integration ppt”
NEET Biology Notes For Chemical Coordination And Integration Hypothalamus
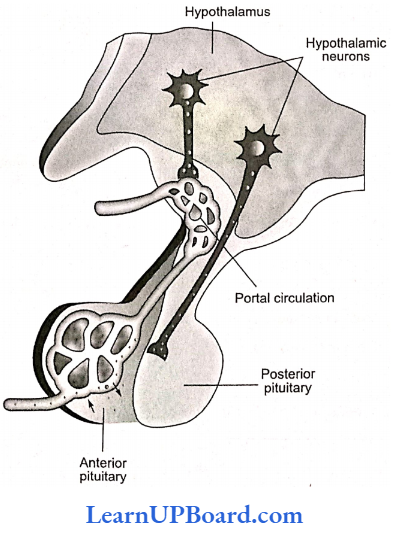
It is the major integrating link between the nervous and endocrine systems. It is the basal part of the diencephalon and contains several groups of neurosecretory cells called nuclei which produce hormones.
- The hormones are of two types, releasing hormones (which stimulate secretion of pituitary hormones) and inhibiting hormones (which inhibit secretions of pituitary hormones).
- These hormones reach the anterior pituitary lobe through the hypophysial portal system.
- The posterior pituitary is under the direct neural regulation of the hypothalamus.
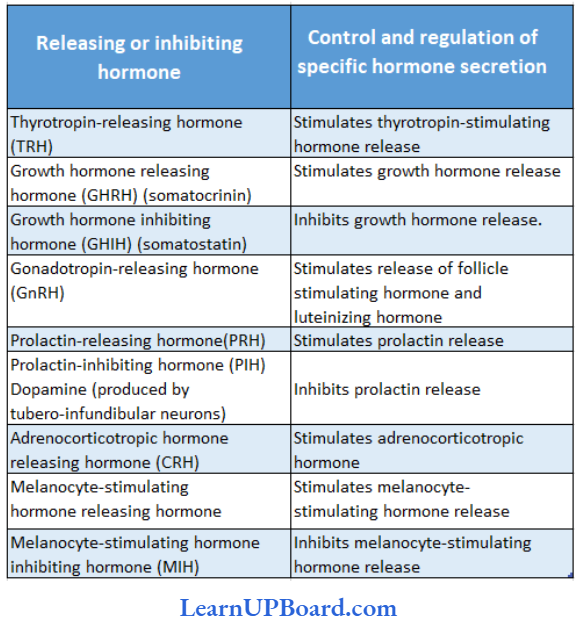
Releasing or inhibiting hormones of the hypothalamus and their roles, factors, and specific hormones they control:
NEET Biology Notes For Chemical Coordination And Integration Hypothalamus Points To Remember
Supra optic nuclei of the hypothalamus secrete the hormone vasopressin whereas paraventricular nuclei secrete the hormone oxytocin.
NEET Biology Notes For Chemical Coordination And Integration Pituitary Gland
It is a pink-colored pea-sized gland about 1.3 cm in diameter and weighs only 0.5 g.
- It is located in a bony cavity called sella turcica of the sphenoid bone and is attached to the hypothalamus via the infundibulum.
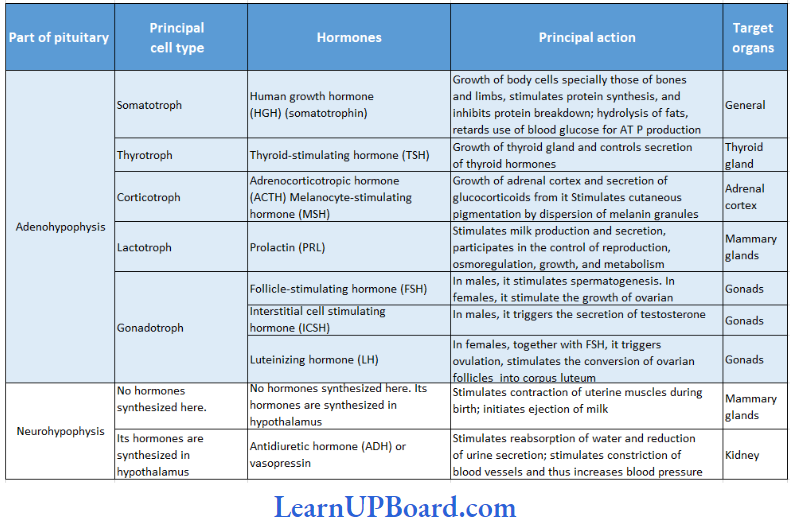
- The pituitary gland has two anatomically and functionally separate lobes—the much larger anterior lobe or adenohypophysis and the posterior lobe or neurohypophysis.
- Adenohypophysis consists of two portions—pars dis-tails and pars intermedia.
- Pars distalis produces a cluster of hormones whereas pars intermedia secretes only one hormone called melanocyte-stimulating hormone (MSH). However, in humans, pars intermedia atrophies and merges with pars distalis during fetal development.
Hormones Of Pituitary Gland And Their Action On Target Organs:
NEET Biology Notes For Chemical Coordination And Integration Pituitary Gland Points To Remember
GH is the only adenohypophysis hormone that is linked directly to the body whereas other adenohypophysis hormones mostly control other glands.
- GH stimulates hepatocytes to release glucose into the blood. In this respect, GH is an insulin antagonist and, thus, can be related to having a diabetogenic effect.
- Pitocin is a synthetic oxytocin which is often given to induce labor.
Disorders Related to GH
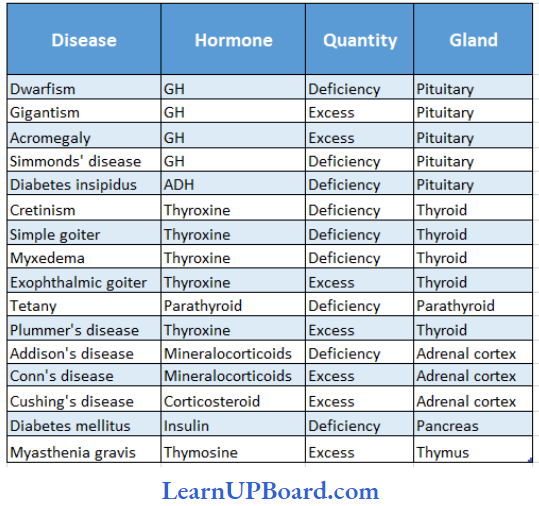
Dwarfism: The failure of secretion of growth hormone from an early age stops the growth of long bones and the body prematurely; this makes the patient dwarf.
Gigantism: On the other hand, excessive secretion of this hormone from childhood turns the patient into a giant with abnormal elongation of all long bones.
Acromegaly: Over secretion of the growth hormone after adolescence causes abnormal elongation of long bones of arms, hands, legs, and lower jaw, and a gorilla-like appearance, but no giant stature.
Hormones of Posterior Pituitary: The posterior pituitary releases two hormones—vasopressin and oxytocin.
- They are synthesized in some hypothalamic neurons and remain stored in their axon terminals inside the posterior lobe called herring bodies.
- Nerve impulses that propagate along the axon and reach axon terminals trigger exocytosis of the secretory vesicles storing these hormones.
“chapter 22 biology class 11 notes “
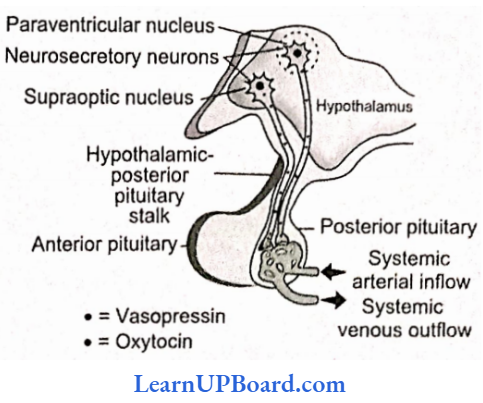
Vasopressin: Whenever the blood osmotic pressure rises due to the loss of water from the body, these neurons are stimulated to release vasopressin into the blood in the posterior lobe.
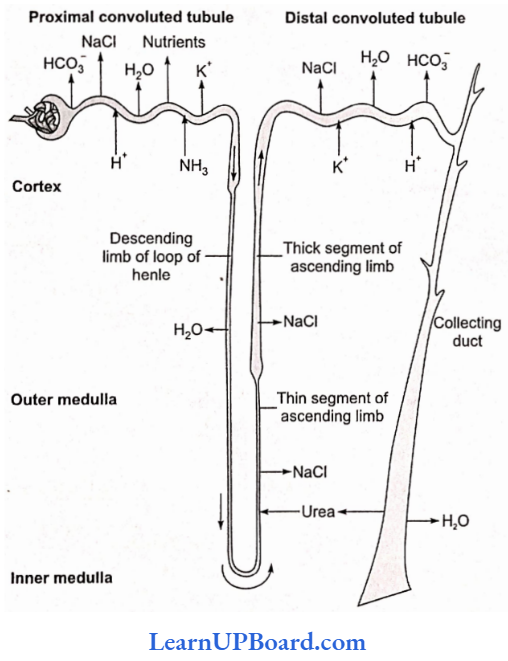
- Vasopressin is also known as ADH because it reduces the volume of urine by increasing the reabsorption of water from the urine in the distal convoluted tubules, collecting tubules, and collection ducts in the kidney. This is done by rendering the walls of those tubules permeable to water.
- Failure of secretion of vasopressin leads to reduced renal reabsorption of water and consequent elimination of a large volume of dilute (hypotonic) urine; this disease is known as diabetes insipidus. Although the volume of wine is increased, no glucose appears in the urine of such patients.
- Besides its antidiuretic effect of reducing the urinary volume, vasopressin also enhances arterial blood pressure by causing constriction or narrowing of arteries.
Oxytocin (Pitocin): The other posterior lobe hormone, viz., oxytocin is secreted into the blood when the hypothalamic neurons are stimulated either due to the distension of the uterus by the full-term fetus or due to the sucking of the breast by the infant.
- Oxytocin contracts the smooth muscles of the uterus and mammary glands. Uterine contractions, stimulated by oxytocin at the end of pregnancy, help in childbirth.
- The oxytocin-induced contractions of the mammary gland muscles help in the flow of stored milk from the mammary gland to the mouth of a suckling infant.
- Even the sight and sound of a baby can cause a nursing mother to secrete this hormone. That is why oxytocin is also called “milk ejection hormone” and “birth hormone.”
NEET Biology Notes For Chemical Coordination And Integration Parathyroids
These are four small pea-sized glands situated very close to the thyroid. They secrete a hormone called parathormone (Collip’s hormone).
- They are under the feedback control of blood calcium levels.
- A fall in blood calcium stimulates them to secrete parathormone and vice versa.
- Parathormone increases the concentration of calcium ions in the blood plasma because it mobilizes more calcium from the bones to the plasma and reduces urinary elimination of calcium.
- It is secreted whenever the plasma Ca2+ concentration falls and restores the Ca2+ concentration to normal in the plasma. On the other hand, it increases phosphate elimination in the urine and consequently lowers the phosphate concentration in the plasma. Thus, parathormone regulates the metabolism of calcium and phosphorus.
Calcium Homeostasis: A higher-than-normal level of calcium ions (Ca2+ ) in the blood stimulates the parafollicular cells of the thyroid gland. They release more calcitonin as the blood Ca2+ level rises.
- Calcitonin promotes the deposition of blood Ca2t into the matrix of bone tissue. This decreases blood Ca2+ levels.
- A lower-than-normal level of Ca2+ in the blood stimulates principal cells of the parathyroid gland.
- They release more parathyroid hormone (PTH) as the blood Ca2+ level falls.
- PTH promotes the release of Ca2+ from the bone matrix into the blood and retards the loss of Ca2+ in the urine. These actions help raise the blood level of Ca2+.
- PTH also stimulates kidneys to release another hormone called calcitriol.
- Calcitriol stimulates increased absorption of Ca2+ from foods in the gastrointestinal tract, which helps increase the blood level of Ca2+.
Disorders Related to Parathyroid
Hypoparathyroidism (parathyroid tetany): If the parathyroids fail to secrete a sufficient amount of parathormone, the concentration of calcium ions falls abnormally in the plasma.
- This increases the excitability of nerves and muscles due to the deficiency of Ca2+ which causes depolarization without usual stimulus. Consequently, sustained contractions (tetany) of the muscles of the larynx, face, hands, and feet are produced.
- This disease is called parathyroid tetany. It can also develop due to accidental damage to the parathyroid or the blood supply during thyroidectomy surgery.
Hyperparathyroidism: The parathyroid tumors secrete excessive amount of parathormone, which causes increased mobilization of bone minerals into the blood, softening of bones, rise in the concentration of calcium ions in the plasma, and deposition of calcium in kidney tubules and other soft tissues. It may cause osteitis fibrosa cystica.
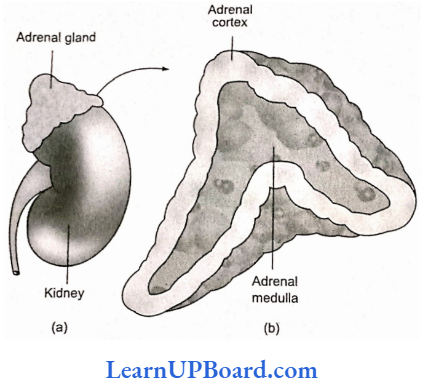
NEET Biology Notes For Chemical Coordination And Integration Adrenal Gland
Adrenals arc two conical pyramid-shaped glands, one immediately above each kidney. Each adrenal is made up of an outer layer mesodermal in origin called the adrenal cortex and a central portion ectodermal in origin called the adrenal medulla.
Adrenal Cortex
This part of the adrenal is vitally important for life, and its destruction or removal kills the animal. It secretes three groups of hormones, viz., mineralocorticoids, glucocorticoids, and sex corticoids.
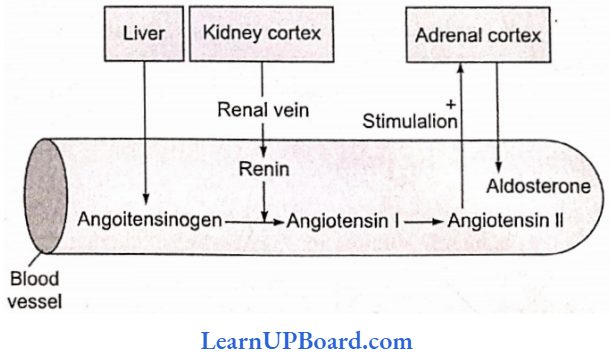
- Mineralocorticoids are secreted from the outermost cellular layer zona glomerulosa of the adrenal cortex. Aldosterone is the principal mineralocorticoid in man, other mammals, and birds.
- Mineralocorticoids regulate the metabolisms of sodium and potassium. Then- secretion is stimulated by a fall in plasma Na+ concentration or a fall in the circulating volume of blood.
- Aldosterone reduces the elimination of Na+ in the urine, sweat, saliva, and bile by enhancing the active reabsorption of this ion from those fluids. It also increases the elimination of K+ in those fluids in exchange for the reabsorbed Na+.
- By retaining more Na+ in the blood, it increases the reabsorption of water from the urine by the osmotic effect of Na+. Due to the same reason, it increases the volumes of blood and other extracellular fluids.
- Glucocorticoids such as cortisol are secreted from the middle cellular layer (zona fasciculata) of the adrenal cortex. Glucocorticoids stimulate gluconeogenesis, ipolysis, and proteolysis and inhibit cellular uptake and utilization of amino acids.
- Cortisol is also involved in maintaining the cardiovascular system as well as kidney functions. The anterior pituitary hormone called corticotropin stimulates glucocorticoid secretion; glucocorticoids, on the other hand, exert a feedback inhibitory effect on corticotropin secretion.
- Glucocorticoids are also anti-inflammatory as they act as the stabilizer of lysosomes of phagocytic cells. Prolonged use of glucocorticoids suppresses the immune response.
- Sex corticoids are secreted from both the middle and inner layers (zona reticularis) of the adrenal cortex. Their secretion is believed to be stimulated by corticotropin of the anterior pituitary.
- They include steroids which may stimulate the development of external sex characters of the male type such as the male pattern and distribution of body hair (role in the growth of axial hair, pubic hair, and facial hair during puberty).
- Examples of sex corticoids are arc androstenedione, dehydroepiandroster, and estrogens.
NEET Biology Notes For Chemical Coordination And Integration Adrenal Gland Points To Remember
- Glucocorticoids include three main hormones: cortisol, corticosterone, and cortisone. Of the three, cortisol is the most abundant (about 95%).
- Glucocorticoids are immunosuppressive, hence also used in transplantation surgery to avoid tissue rejection by the immune system of the recipient.
- Zona fasciculata is the widest layer of the adrenal cortex.
Disorders Related to Adrenal Cortex
- Addison’s disease: A destruction of the adrenal cortex by diseases such as tuberculosis produces Addison’s disease due to the deficiency of both glucocorticoids and mineralocorticoids. Symptoms include a bronze-like pigmentation of the skin, low blood sugar, low plasma Na+, high plasma K+, increased urinary Na+, nausea, vomiting, and diarrhea.
- Cushing’s syndrome: A tumor of the adrenal cortex may secrete too much cortisol to produce Cushing’s syndrome. High blood sugar, appearance of sugar in the urine, obesity, wasting of limb muscle, rise in plasma Na+, fall in plasma K+ rise in blood volume, and high blood pressure are observed in the patient.
- Aldosteronism (Conn’s syndrome): An excessive secretion of aldosterone from an adrenal cortical tumor produces aldosteronism. This disease is characterized by high plasma Na+, low plasma K+, rise in blood volume, and high blood pressure.
- Adrenal virilism: An excessive secretion of sex corticoids produces the male-type external sex characters such as beard, mustache, and male voice in women. The disease is called adrenal virilism.
“ch 22 biology class 11 notes “
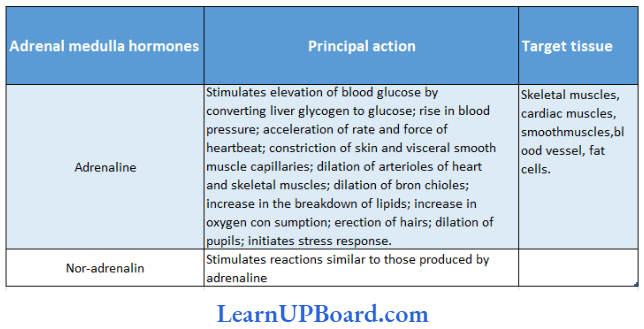
Adrenal Medulla: The adrenal medulla helps the body to combat stress or emergency conditions.
- But it is not vital for survival and may be removed without causing death.
- The adrenal medulla secretes two hormones, viz. adrenaline and nor-adrenaline.
- The proportion of the two hormones varies from species to species; in man, much more adrenaline is secreted than nor-adrenaline.
- The secretion of these hormones is stimulated when nerve impulses reach the adrenal medulla through sympathetic nerve fibers.
- These hormones act on organs and tissues supplied by sympathetic fibers and produce effects like those of sympathetic stimulation.
- Nor-adrenaline is also released at sympathetic nerve terminals to transmit nerve impulses from them to smooth muscles and glands.
- Both sympathetic nerves and adrenal medulla are stimulated by physical stress such as a fall in blood pressure or blood sugar, pain, cold, or injury; both are also stimulated by emotional stress such as anger, fear, and grief.
- All these indicate that the adrenal medulla and sympathetic nervous system function as a closely integrated system; this may be called the sympathetic-adrenal system and is another instance of close coordination between nerves and hormones.
Hormones Of Adrenal Medulla And Their Action:
NEET Biology Notes For Chemical Coordination And Integration Pancreas
The pancreas comprises both exocrine and endocrine parts. The endocrine part consists of small masses of hormone-secreting cells called islets of Langerhans.
Different Types Of Pancreatic Cells And Their Action:
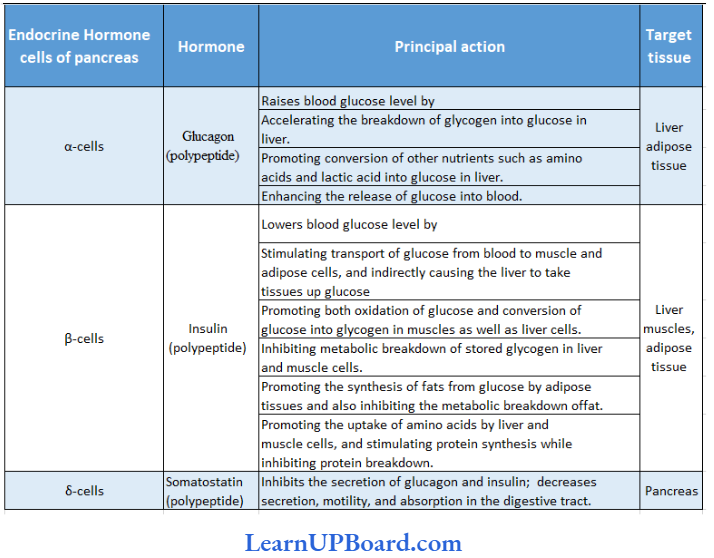
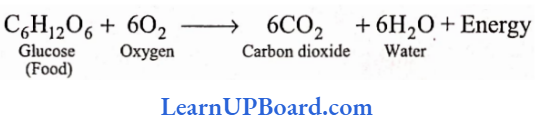
Disorders related to irregular insulin secretion: Failure of insulin secretion produces diabetes mellitus. In this disease, the Hood sugar remains abnormally high and exceeds the renal threshold for vorticose. Consequently, glucose appears in the urine (glucosuria).
- The utilization of glucose is decreased: instead, the catabolism of fats and proteins arc enhanced. Increased oxidation of fat produces ketone bodies such as acetoacetate and acetone. Also, the blood cholesterol rises.
- The osmotic effect of glucose in the urine considerably increases the volume of urine (polyuria). Thirst is enhanced due to urinary loss of water.
- Injuries take a long tune to heal and may turn into gangrenes. In extreme cases, the patient suffers from coma and may die. Administration of insulin reduces the blood sugar and checks oilier symptoms of diabetes.
NEET Biology Notes For Chemical Coordination And Integration Pancreas Points To Remember
Diabetes mellitus (type 1): It is known as insulin-dependent diabetes mellitus (IDDM) and is also known as juvenile-onset diabetes because it most commonly develops in people younger than 20. It is an autoimmune disorder in which the immune system destroys β-cells.
Diabetes mellitus (type 2): It is known as non-insulin-dependent diabetes mellitus (NIDDM). It is also known as maturity-onset diabetes because it occurs later in life. It arises not from the shortage of insulin but because of target cells which become less sensitive to insulin.
NEET Biology Notes For Chemical Coordination And Integration Pineal Gland And Its Hormones
The pineal gland is regarded as the vestige of the third eye as well as a functional endocrine gland.
- It is attached to the roof of the third ventricle in the rear portion of the brain, ectodermal in origin, and is known as the pineal gland, named for its resemblance to a pine cone.
- It has no direct connection with the central nervous system.
- It is variable in size and weighs about 150 mg, but is richly vascularized and secretes several hormones, including melatonin.
- In humans, it has no light-sensitive cells, but in lower vertebrates, the pineal gland is cye-like and responds to light.
- The pineal gland functions as a biological clock and a neurosecretory transducer, converting neural information.
- More melatonin is produced during darkness.
- Its formation is interrupted when light enters the eyes and stimulates tire retinal neurons.
- They transmit impulses to the hypothalamus, and finally to the pineal gland.
- The result is inhibition of melatonin secretion.
- In this way, the release of melatonin is governed bv the diurnal dark-light cycle.
- Melatonin also influences body temperature and metabolism. pigmentation, menstrual cycle, and defense capability.
NEET Biology Notes For Chemical Coordination And Integration Thymus
It is a soft, bilobed structure, where the two lobes lie side by side and are joined in the middle by connective tissue.
- It is pyramidal in children with a maximum size reaching about 15 years of age.
- Its size is reduced somewhat later due to a decrease in its lymphoid content.
- The weight of the thymus at birth is 15-20 g in children remaining at that level thereafter.
- It is deep red at a young age. becoming thinner and greyer with age. and later yellowish due to infiltration of adipose tissue.
- The thymus is covered on the outside by a capsule of loose connective tissue which also penetrates the interior of the gland forming septa and irregular lobules.
- There is an outer cortex of densely packed thymocytes (or T-lymphocyte lineage) and an inner medulla having connective tissue with fewer lymphoid cells.
- The balls of flattened epithelial cells called HassaTs corpuscles occur here and there in the medulla.
- Thymocytes also occur along with some B-lympho- cytes.
- The hormone produced by the thymus gland is called thymosin.
- Thymosin released in the bloodstream has a stimulating effect on the entire immune system.
- It promotes the proliferation and maturation of T-lym-phocytes. It is also called “the throne of immunity” or “training school of T-lymphocytes.”
NEET Biology Notes For Chemical Coordination And Integration Thymus Points To Remember
Thymosin plays a major role in the differentiation of T-lymphocytes which provide cell-mediated immunity. These also promote the production of antibodies to pros ide humoral immunity
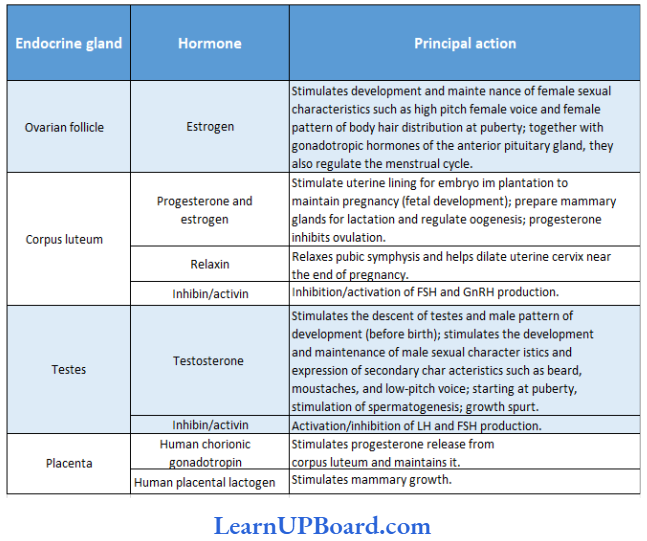
NEET Biology Notes For Chemical Coordination And Integration Sex Hormones And Their Functions
Testes in males and ovaries in females secrete sex hormones at puberty.
Hypogonadism: Defects in. or injury to. the hypothalamus, pituitary, testes, or ovary result in hypogonadism.
- Male hypogonadism can consist of deficient androgen production (hypofunction of Leydig cell) deficient sperm formation (hypofunction of Sertoli cell) or both before puberty.
- It results in the lack of development of secondary sexual characteristics and male musculature.
- Female hypogonadism results from the hyposecretion of estrogen, resulting in the cessation of reproductive cycles. Such hypogonadism can result from a shortage of pituitary gonadotropins (LH, FSH, or both) or can represent primary testicular/ovary failure.
Precocious Puberty: True sexual precocity, i.e., the early maturation of ovaries and testes with the production of ova before the age of nine years in girls or the production of sperm before 10 years in boys occurs without evident cause.
- Sexual pseudoprecocity results from excesses of sex hormones from the adrenal cortex, testis, ovary, or from other sources, including extragonadal tumors.
- Sexual pseduoprecocity in boys occurs as a consequence of excess testosterone produced by the tumors of the testis or adrenals. In such cases, enlargement of the penis, accelerated appearance of sexual characteristics such as pubic and axillary hair, masculinization, faster body growth, and ultimate stunting are present.
- Sexual pseudo-precocity in girls arises from an increased supply of estrogen secreted by tumors of the ovaries or adrenals.
- The external manifestations of sexual maturation, for example, breast formation and appearance of pubic hair, appear early, but the maturation and discharge of ova do not occur.
Hormones Regulating Reproduction:
Eunuchoidism: Eunuchoidism results from the failure of testosterone secretion.
- For this disorder, secondary sex organs such as the prostate gland, seminal vesicles, and penis remain infantile and small in size and fail to function.
- Spermatozoa fail to be produced.
- External sex characters such as beards, mustaches, and low-pitched male voices fail to develop.
NEET Biology Notes For Chemical Coordination And Integration Gynecomastia
Gynecomastia is the development of breast tissue in males and is usually due to the perturbation of the gen-to-androgen ratio.
- In the neonatal period and during puberty, gynecomastia is due to a temporary increase in circulating estrogen.
- Decreased testosterone in later life may also lead to gynecomastia.
- Removal of testes in males is called castration.
- It will lead to a decline in the androgen level and secondary characters fail to appear.
- It can lead to the retention of a high-pitched juvenile voice in a male.
“ch 22 bio class 11 notes “
NEET Biology Notes For Chemical Coordination And Integration Hormones Of Heart, Kidney, And Gastrointestinal Tract
In addition to endocrine glands, hormones are also secreted by some tissues which are not endocrine glands. For example,
- The atrial wall of the heart secretes an important peptide hormone called atrial natriuretic factor (ANF) which decreases blood pressure. When blood pressure is increased. ANF is secreted which causes dilation of blood vessels. This reduces the blood pressure. Juxtaglomerular cells of the kidney produce a peptide hormone called erythropoietin which stimulates poiesis (formation of RBC).
- Endocrine cells present in the different parts of the gastrointestinal tract secrete four major peptide hormones, viz., gastrin, secretin, cholecystokinin (CCK), and gastric inhibitory peptide (mentioned in animal nutrition).
NEET Biology Notes For Chemical Coordination And Integration Molecular Mechanism Of Hormone Action
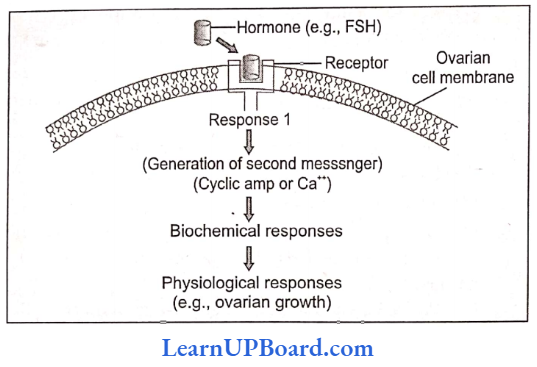
Catecholamines, peptides, and protein hormones are not lipid-soluble, and so cannot enter their target cells through the bilipid layer of the plasma membrane.
- Instead, these water-soluble hormones interact with a surface receptor, usually a glycoprotein, and, thus, initiate a chain of events within it.
- The hormone insulin provides a well-studied example.
Extracellular receptor: The membrane-bound receptors of insulin are heterotetrameric proteins consisting of four subunits, two a-subunits protrude out from the surface of the cell and bind insulin, and two β-subunits that span the membrane and protrude into the cytoplasm.
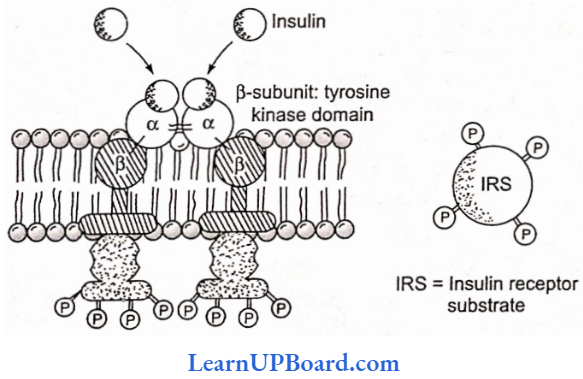
Binding to the receptor: The binding of insulin to the outer subunits of the receptor causes a conformational change in the membrane-spanning β-subunits, which is also an enzyme, a tyrosine kinase. The activated β-subunits add phosphate groups of specific tyrosine residues located in the cytoplasmic domain of the receptor as well as a variety of insulin receptor substrates.
Secondary messengers (mediator): As a result of β-subunit activity, a transducer G-protein activates the enzyme phosphodiesterase. This enzyme breaks phosphatidylinositol 4,5-bishops-phase (PIP2) into a pair of mediators: inositol triphosphate (IP3) and diacylglycerol (DG). In turn, IP3, which is water-soluble diffuses into cytoplasm and triggers the release of another messenger, Ca2+ ions, for intracellular calcium-mediated processes, while DG remains v/ithin the membrane where it activates-, an enzyme called protein kinase C. which in turn, activates many other enzymes such as pyruvate dehydrogenase, and so brine. about the physiological effects.
Antagonistic effect: Many cells use more than one secondary messenger.
- In heart cells, cAMP serves as a secondary messenger, speeding up muscle cell contraction in response to adrenaline, while cyclic guanosine monophosphate (cGMP) serves as another secondary messenger, slowing muscle contraction in response to acetylcholine.
- It is in this way that the sympathetic and parasympathetic nervous systems achieve antagonistic effects on the heartbeat.
- Another example of an antagonistic effect is insulin, which lowers blood sugar levels, and glucagon, which raises it.
Synergistic effect: Another type of hormonal interaction is known as synergistic effect. Here, two or more hormones complement each other’s actions and both are needed for full expression of the hormone effects. For example, the production, secretion, and ejection of milk by mammary glands require the synergistic effect of estrogens, progesterone, prolactin, and oxytocin.
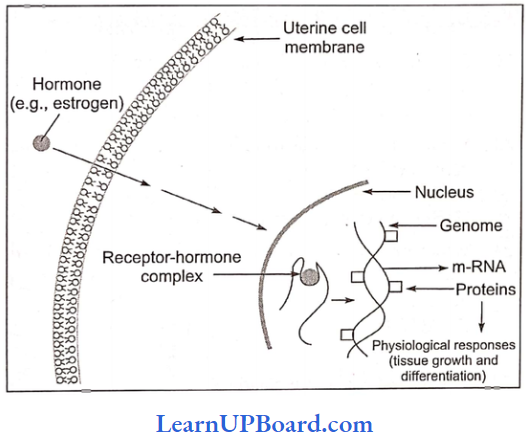
Intracellular receptors: Unlikely catecholamine and peptide hormones, steroid and thyroid hormones are lipid-soluble hormones and readily pass through the plasma membrane of a target cell into the cytoplasm.
- There they bind to specific intracellular receptor proteins, forming a complex that enters the nucleus and binds to specific regulatory sites on chromosomes.
- The binding alters the pattern of gene expression, initiating the transcription of some genes (DMA) while repressing the transcription of others. This results in the production of specific mRNA translation products, proteins, and usually enzymes.
- The actions of lipid-soluble hormones are slower and last longer than the actions of water-soluble hormones. These cause physiological responses that are characteristic of the steroid hormones.
Disease Caused By Hormonal Irregularities:
NEET Biology Notes For Chemical Coordination And Integration Chemical Coordination And Integration Assertion-Reasoning Questions
In the following questions, an Assertion (A) is followed by a corresponding Reason (R). Mark the correct answer.
- If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
- If both Assertion and Reason are true, but the Reason is not the correct explanation of the
Assertion. - If Assertion is true, but Reason is false.
- If both Assertion and Reason are false.
Question 1.
Assertion: Diabetes insipidus is marked by excessive urination and too much thirst for water.
Reason: Anti-diuretic hormone (ADH) is released by the posterior lobe of the pituitary gland.
Answer: 2. If both Assertion and Reason are true, but the Reason is not the correct explanation of the
Assertion.
Question 2.
Assertion: Insulin is not given orally.
Reason: Insulin hormone is lipid-soluble and directly enters inside the cell membrane.
Answer: 3. If Assertion is true, but Reason is false.
Question 3.
Assertion: Chorionic gonadotrophin prevents corpus luteum from involuting.
Reason: It has a property similar to luteinizing hormone.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 4.
Assertion: Thyroxine shows a calorigenic effect.
Reason: Thyroxine increases catabolism, produces energy, and increases body temperature.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 5.Assertion: Inhibin is secreted by the corpus luteum.
Reason: They inhibit the FSH and GnRH production.
Answer: 2. If both Assertion and Reason are true, but the Reason is not the correct explanation of the Assertion.
Question 6.Assertion: Adrenal glands have dual origin.
Reason: The adrenal cortex develops from the endoderm while the adrenal medulla develops from the mesoderm.
Answer: 3. If Assertion is true, but Reason is false.
Question 7.
Assertion: Vasopressin is also called an antidiuretic hormone.
Reason: Vasopressin reduces the loss of water in urine by increasing water reabsorption in nephrons.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 8.
Assertion: Oxytocin is also known as anti-diuretic hormone (ADH).
Reason: Oxytocin can cause an increase in the renal reabsorption of water.
Answer: 4. If both Assertion and Reason are false.
Question 9.
Assertion: The failure of secretion of the hormone vasopressin causes diabetes mellitus in the
patient.
Reason: Vasopressin reduces the volume of urine by increasing the reabsorption of water from the urine.
Answer: 4. If both Assertion and Reason are false.
Question 10.
Assertion: The adrenal cortex is called the gland for “fight, fright, and flight.”
Reason: The hormones adrenaline and nor-adrenaline help the body combat stress and emergency conditions.
Answer: 4. If both Assertion and Reason are false.