NEET Biology Notes Excretory Products And Their Elimination Introduction
The process of removal of metabolic wastes from the body is called excretion. The regulation of its solute and water movements by osmosis is done in two ways:
- Osmoconformers are animals that do not actively control the osmotic concentration of their body fluids. They rather change the osmolarity of body fluids according to the osmolarity of the surrounding medium.
- All marine invertebrates and some freshwater invertebrates are strictly osmoconformers. Hagfish is a vertebrate osmoconfonner. Osmoconformers show an excellent ability to tolerate a wide range of cellular osmotic environments.
- Osmoregulators, on the other hand, are the animals that maintain an internal osmolarity, different from the surrounding medium in which they inhabit. Many aquatic invertebrates are strict or limited osmoregulators. Most vertebrates are strict osmoregulators, i.e., they maintain the composition of the body fluids within a narrow osmotic range.
- The notable exceptions, however, are the hagfish (.Myxirte sp., a marine cyclos- tome fish) and elasmobranch fish (sharks and rays). Osmoregulators must either eliminate excess water if they are in a hypotonic medium or continuously take in water to compensate for water loss if they are in a hypertonic solution. Therefore, osmoregulators have to spend energy to move water in or out and maintain osmotic gradients by manipulating solute concentrations in their body fluids.
excretion and elimination class 11
NEET Biology Notes Excretory Products And Their Elimination Water And Solute Regulation In Different Environments
Fresh Water Environment: The osmolarity of fresh water is generally much less than 50 mosm/L while the freshwater vertebrates have blood osmolarities in the range of 200-300 mosm/L.
- The body fluids of freshwater animals are generally hypertonic to their surrounding environment.
- The problems faced by the animals are:
- Loss of body salt to the outside
- Entry of excess water
- Protozoa (Amoeba, Paramecium) have contractile vacuoles that pump out excess water.
- Adaptations shown by other animals include
- To minimize the loss of water and salts by specialized body cover in the form of scales or adipose cover.
- Lesser intake of water in order to reduce the need to expel excess water.
- Passing out highly dilute urine, o Presence of monocytes or chloride cells which can actively uptake the salts (Na+ and Cl–) from the surrounding water (surrounding water has less than 1 mm NaCI and plasma concentration has more than 100 mm, therefore uptaken actively).
Read and Learn More NEET Biology Notes
Marine Environment: Sea water usually has an osmolarity of about 1000 mm/L. The osmolarity of human blood is about 300 mm/L.
- The osmoregulatory problems in marine situations are opposite to those in freshwater environments.
- Marine bony fishes have body fluids hypotonic to seawater, and thereby, they tend to lose water from the body through permeable surfaces (gill membranes, oral and anal membranes).
- To compensate for the water loss, marine bony fishes drink seawater. However, drinking seawater results in a gain of excess salts.
- The monocytes or chloride cells of the gill membrane of marine bony fish help to eliminate excess monovalent ions from the body fluid to the seawater.
- Divalent cations are generally eliminated through fecal matter.
- In general, the body fluids of marine invertebrates, ascidians, and hagfish are isosmotic to seawater.
- The osmolarity of body fluids is raised by accumulating certain organic substances (osmolytes).
- Retention of osmolytes in body fluids reduces the osmoregulatory challenges.
- The best-known examples of such organic osmolytes are urea and trimethylamine oxide (TMAO).
NEET Biology Notes Excretory Products And Their Elimination Excretory Products And Their Elimination Point To Remember
The body fluids of sharks and coelacanths are slightly hyperosmotic to seawater due to retention of urea and TMAO while hypotonic to seawater as they maintain far lower concentrations of inorganic ions in the body fluids.
Terrestrial Environment: Humans, for example, die if they lose around 12% of their body water. Therefore, water loss must be compensated by drinking and eating moist food.
- Desert mammals are well adapted to minimize water loss. Kangaroo rats, for example, lose so little water that they can recover 90% of the loss by using metabolic water (water derived from different cellular metabolic processes). The nasal countercurrent mechanism for conserving respiratory moisture is also important.
- When water is not available, dead camels do not produce urine but store urea in tissues and solely depend on metabolic water. When water is available, they rc- hydrate themselves by drinking up to So L of water in 10 min.
NEET Biology Notes Excretory Products And Their Elimination Types Of Nitrogenous Waste Products In Animal World
Excretion is the removal of metabolic wastes from the body. The removal of undigested food is called detecation or egestion. Carbon dioxide and water are metabolic wastes of carbohydrate and fat metabolism. Their removal is. therefore, excretion.
- Ammonia: It is the first metabolic waste of protein metabolism. Ammonia is produced in the liver by the process of deamination. Ammonia is very toxic and requires a large amount of water for its excretion.
- Urea: It is a white crystalline solid produced in the liver from NH3 and CO2, It is comparatively less toxic. If we take more proteins, more urea is excreted out. Normal blood urea level is 18-38 mg/100 mL of blood.
- Uric Acid: It is produced in the liver. It can be excreted in semisolid or crystalline form. The excretion of uric acid in crystalline form is helpful in the conservation of body water. Bird droppings (guano) consist of uric acid and phosphate-rich feces.
- Xanthines and guanines: These are metabolic wastes of nucleotide metabolism. These are found in spiders and penguins.
- Trimethylamine oxide: It is found in marine bony fish.
- Ornithuric acid: It is a specialized product in the excretion of birds.
- Hippuric acid: It is a specialized product in the excretion of mammals. It is produced from benzoic acid.
- Creatinine: It is produced from creatine phosphate present in muscles. An increased level of creatinine is indicative of kidney damage.
Animals are classified on the basis of their main excretory product. They could be of the following types:
Ammonotelic Animals: The excretory product is mainly ammonia.
- Ammonia molecules, being readily soluble in water, easily cross the membrane barriers.
- In soft-bodied invertebrates, it diffuses out across the whole body surface while in fishes such as NH4+ or ammonium ions across gill epithelium, e.g., aquatic invertebrates such as Amoeba, and sponges. Hydra. crayfish, starfish, tadpole larvae of frogs, and bony fish.
Ureotelic Animals: The excretory product is mainly urea.
- Urea can be tolerated in much more concentrated form because it is 100,000 times less toxic than ammonia.
- However, the entire amount of urea produced is not excreted out but a part is retained in the kidney and is involved in osmoregulation. For example, cartilaginous fish, amphibians, and mammals.
“excretory class 11 “
Uricotelic Animals: The excretory product is mainly uric acid.
- Uric acid can be passed out almost in the form of a precipitate since it is almost insoluble in water. This leads to minimum loss of water.
- Uricotclism is very important for land vertebrates laying shelled eggs.
- If the embryo within the shelled egg had produced ammonia or urea, that would have accumulated to a toxic level. However, this problem is solved by being uricotelic, as uric acid, being almost insoluble, gets precipitated and remains with the shell only.
- This problem is not faced by fishes or amphibians by have shell-less eggs (ammonia or urea can diffuse out) or mammals (as urea is carried away by maternal blood at the placenta). For example, reptiles, birds, cockroach.
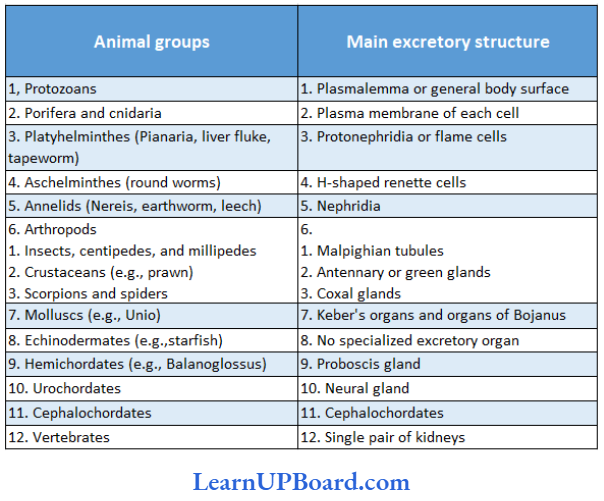
Animal Groups And Their Main Excretory Structures:
NEET Biology Notes Excretory Products And Their Elimination Types Of Kidney
Archinephric kidney: It is also known as the ancestral kidney. Such a kidney is found in the larvae of certain cyclostomes (e.g., Myxine) but does not occur in any adult vertebrate. Glomeruli are only present in some of the posterior tubules. Glomeruli are external (without capsule).
- Pronephric kidney: Ciliated funnels or nephrostomes are present, e.g., tadpoles of frogs and cyclostomes. It is also called the anterior kidney.
- Mesonephric kidney: When Bowman’s capsule is present in the uriniferous tubule, e.g., fish and frog.
- Metanephric kidney: This is the most advanced kidney in which the Loop of Henle is present, e.g., reptiles, birds, and mammals.
NEET Biology Notes Excretory Products And Their Elimination Urea Synthesis (Ornithine Cycle)
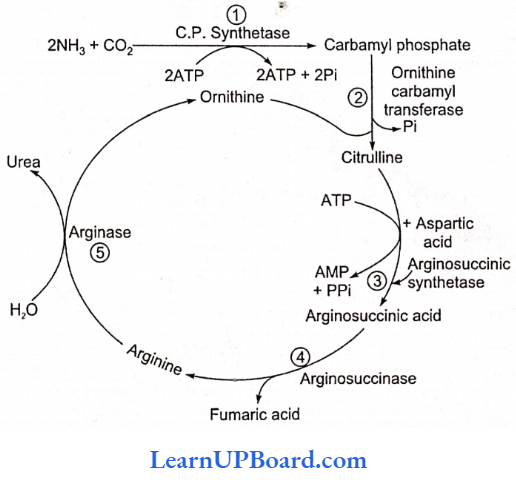
Urea synthesis (ornithine cycle) is the biochemical aspect of excretion. Also called the Krebs-Henseleit cycle, it occurs in the liver and includes:
- The formation of carbamoyl phosphate by the combination of ammonia, CO2, and ATP.
- Carbamoyl phosphate combines with ornithine to form citrulline.
- Citrulline joins aspartic acid and changes to argininosuccinic acid.
- The latter breaks into fumaric acid and arginine.
- With the help of the enzyme arginase, arginine is hydrolyzed to urea and ornithine (which is thus regenerated and re-used in the cycle).
NEET Biology Notes Excretory Products And Their Elimination Human Excretory System
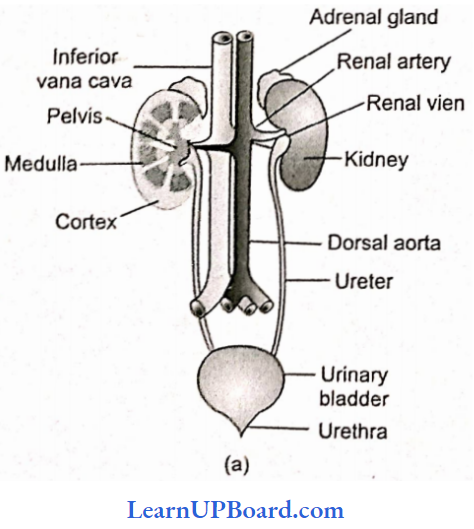
In humans, the excretory system consists of a pair of kidneys, a pair of ureters, a urinary bladder, and a urethra.
Kidneys: Kidneys are reddish brown, bean-shaped structures situated between the level of the last thoracic and third lumbar vertebra close to the dorsal inner wall of the abdominal cavity. Each kidney measures about 10-12 cm long, 5-7 cm in width, and 2-3 cm thick. It weighs about 120-170 g in adults.
- The left kidney sits a little higher than the right one because of more space being occupied by the liver on the right side.
- Towards the center of the inner concave surface of the kidney is a notch called the hilum, through which the ureter, blood vessels, and nerves enter.
- Inner to the hilum is a broad funnel-shaped space called the renal pelvis.
The kidney is covered by three protective layers which are as follows:
- Renal capsule: It is the innermost, tough protective cover made up of white fibrous connective tissue, with few elastic fibers and few muscles.
- Adipose capsule: It is the middle cover involving adipose tissue and acts as a shock absorber.
- Renal fascia: It is the outermost fibrous cover linking the kidneys with the abdominal wall. As the kidneys are fused with the body wall on the dorsal side, the peritoneal cover is present only on the ventral side. This arrangement is called retroperitoneal arrangement.
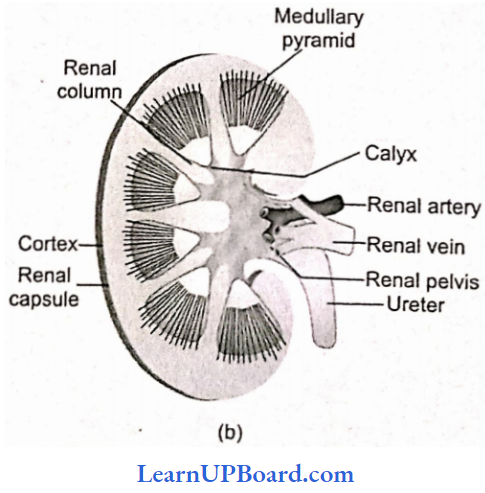
Internal Structure Of Kidney
A longitudinal section of the kidney shows two functional layers the outer renal cortex and the inner renal medulla. Renal cortex: It is the outer part which is dark in color and granular in nature.
Renal medulla: It is the inner part which is lighter in color and striated in nature. The medulla has 8-18 conical renal pyramids. They represent the multilobular condition of the fetal kidney.
- Each renal pyramid has a broad base towards the cortical side. Apex is pointed and is called the renal papilla.
- One to three renal papillae project into an activity called minor calyx, which join up and form major calyces.
- The cortex projects into the medulla in the regions in between the pyramids and calyces, called the renal columns of Bertini.
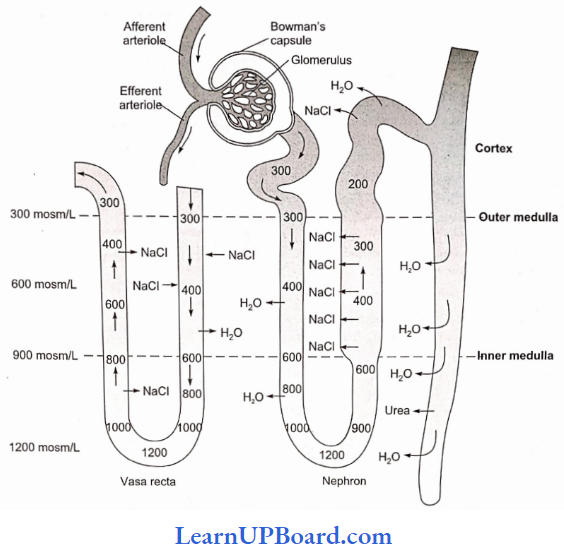
- The interstitial fluid of the medulla region has a higher osmotic concentration equal to some 1200 mosm/L due to a higher quantity of two solutes, NaCl and urea.
- The cortical region close to the medulla is called a juxtamedullary area.
- The major calyces open into a broad funnel-shaped structure called renal pelvis placed inner to the hilum. It is lined by transitional epithelium. It leads into the ureter.
- The structural and functional units of the kidney are called nephrons or uriniferous tubules.
- There are about 1 million nephrons in each kidney.
- The number of uriniferous tubules decreases with age.
Ureters: They are a pair of fine whitish distensible muscular tubes of 25-30 cm in length and about 3 mm in diameter.
“excretory class 11 notes “
- Ureters develop from the hilum part of the kidneys, descend along the abdominal wall, and bend obliquely inward and upward to open into the urinary bladder in the region of trigone by oblique slits, one on each side.
- The wall of the ureter has three coats—external adventitia, middle muscular, and inner mucosa. The muscular coat has three layers of smooth muscle fibers—outer longitudinal, middle circular, and inner longitudinal.
- Ureters are always undergoing peristalsis which helps in passing urine from the kidney to the urinary bladder.
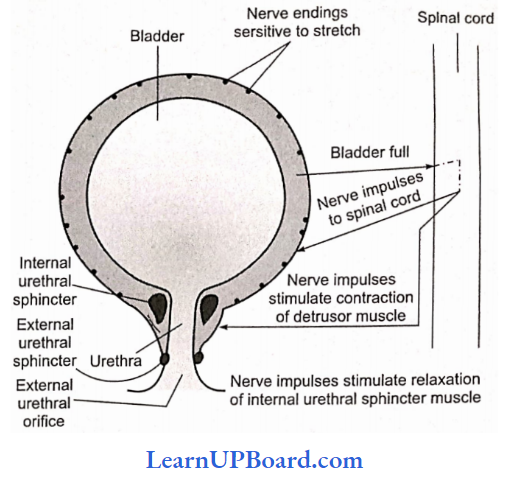
Urinary bladder: It is a median pyriform sac that varies in shape, size, and position according to the amount of urine contained in it.
- The fully distended bladder becomes ovoid in outline.
- The bladder has three parts—apex, fundus or body, and neck. The body has a triangular area called a trigone.
It has openings of ureters and an internal urethral orifice. - The neck region possesses two sphincters, an involuntary internal sphincter and a voluntary external sphincter. The neck leads into the urethra.
- The wall of the urinary bladder consists of three coats— outer adventitia, middle muscular, and inner mucosa.
- The muscle present in the middle muscular coat is also called the detrusor muscle because it takes part in detrusion or pushing down of urine.
- The muscular coat has involuntary circular muscles in the middle and involuntary longitudinal muscles on either side.
- Mucosa has loose connective tissue towards the side of the muscular layer and transitional epithelium or another lean toward the lumen.
- Adventitia is formed of soft connective tissue.
- During the micturition, both the sphincters undergo relaxation.
- The cerebral cortex directs the sphincter to relax and the person undergoes urination.
- The wall of the urinary bladder is innervated by both the sympathetic and parasympathetic nervous systems.
Urethra: Ureter is present only in mammals. It starts from the neck of the urinary bladder and opens outside the body.
- In females, it is short (2-4 cm), straight, and concerned with the release of urine through an aperture called urethral orifice or urinary aperture present in the vulva in front of the vaginal aperture. However, in males, it is quite long (20 cm) and passes through the ejaculatory duct, prostate gland, Cowper’s glands, and penis.
- It is concerned with the release of urine as well as semen (sperms + glandular secretion) through an aperture called urinogenital aperture at the tip of the penis.
Blood Supply To The Kidney: A renal artery enters each kidney and divides into many afferent arterioles which enter Bowman’s capsules and sub-divide to form glomerulus.
- The glomerular capillaries rejoin to form efferent arteriole.
- An efferent arteriole is narrower than an afferent arteriole. This raises blood pressure inside the glomerulus.
- Efferent arteriole further forms numerous peritubular capillaries in the cortex region around the proximal and distal convoluted tubules of the nephron.
- It further forms vasa recta around the loop of Henle.
- Blood from the vasa recta is released into the renal venule from where it escapes into the renal vein.
Types Of Nephrons: A kidney has two types of nephrons—cortical and juxtamedullary. They are held together with the help of connective tissue.
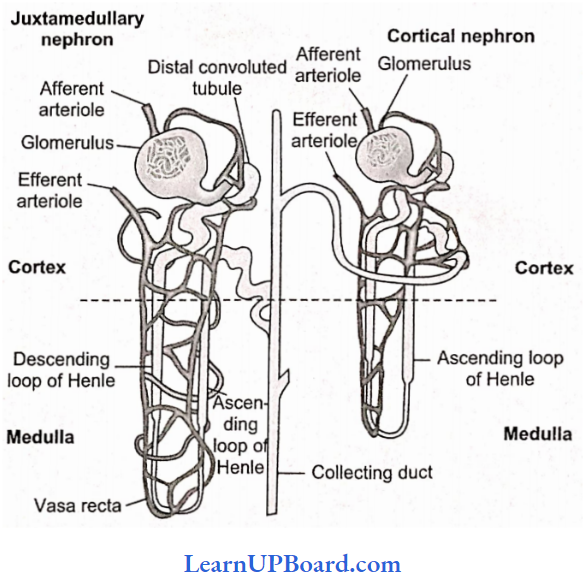
Cortical Nephrons: They constitute about 85% of the total nephrons.
- Cortical nephrons are smaller in size with a major part lying in the cortex.
- The tubule is much coiled.
- The loop of Hcnle is short and extends into the medulla to a short distance.
- Vasa recta are absent or highly reduced.
- Glomeruli lie in the outer cortex.
Juxtamedullary Nephrons: They are approximately 15% of the total nephrons and are present at the junction of the cortex and medulla region of the kidney.
- They have a large size, less coiling, and a long loop of Henle.
- Glomeruli occur in the inner cortex.
- The long loops of Henle are placed deep in the medulla.
- Vasa recta occur over the loops of Henle.
- Juxtamedullary nephrons become active during a shortage of water.
- They increase water reabsorption and, therefore, control the volume of plasma.
- The system usually works under stressful conditions.
Structure Of Nephron: The nephron or uriniferous tubule is the structural and functional unit of the kidney.
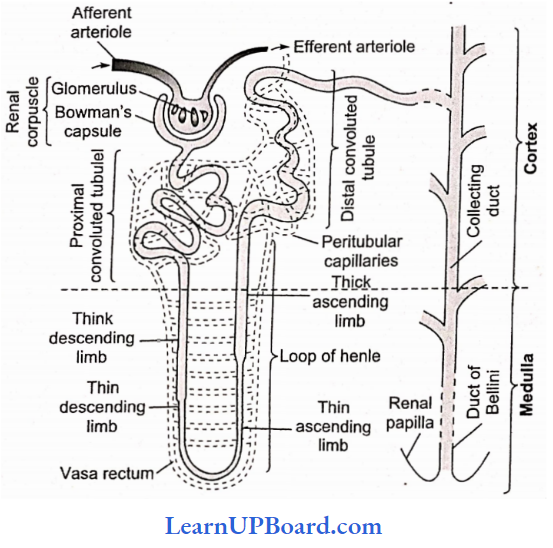
It is about 3 cm long and 20-60 mm in diameter. Each nephron consists of two parts—glomerulus and renal tubule (Bowman’s capsule, PCT, Henle’s loop, and DCT).
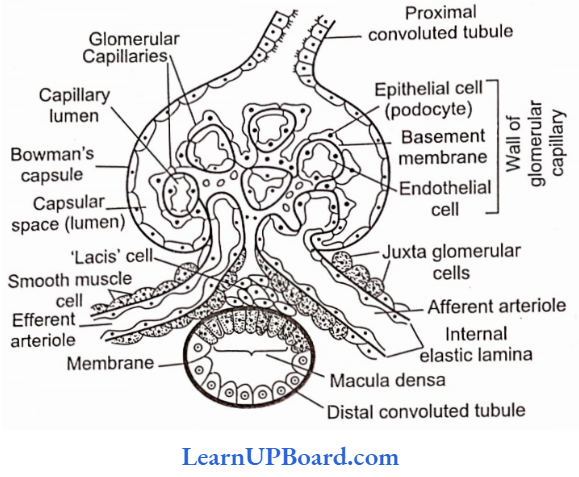
Bowman’s Capsule: It is a blind, double-walled, cup-shaped structure. The two walls of Bowman’s capsule are the inner visceral and outer parietal. Both are single-layered and are supported over a basement membrane.
“excretory products and their elimination ppt “
Visceral layer (inner wall): The inner wall consists of flat squamous epithelial cells on the periphery and specialized podocytes in the remaining part.
- A podocyte has a number of interdigitated evaginations called pedicels or feet.
- The pedicels rest over the basement membrane.
- They enclose slit pores or filtration slits.
- The diameter of these slits is about 25 nm.
- Pedicels also possess contractile filaments which help in the passage of filtrate through the filtration slits.
Parietal layer (outer wall): The outer wall consists of flat squamous epithelium. The space between the two layers of Bowman’s capsule is called lumen or capsular space.
Glomerulus: The glomerulus is a tuft of capillaries formed by fine blood. vessels lying in the Bowman’s capsule.
- The glomerulus receives blood from an afferent arteriole.
- Blood is taken away from the glomerulus by an efferent arteriole.
- The latter has a narrower diameter than that of the afferent arteriole.
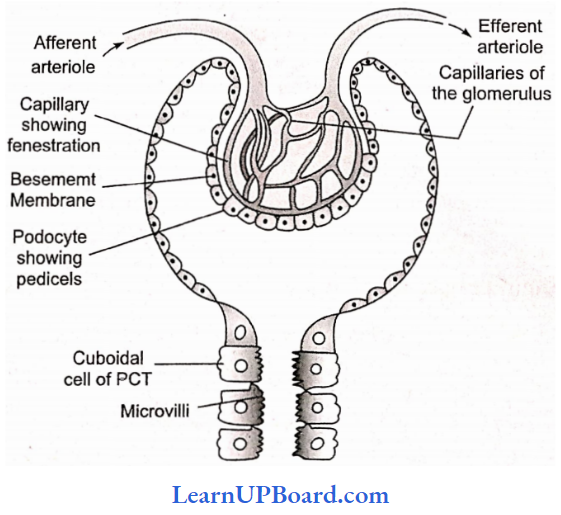
- Blood vessels of glomerulus arc similar to those of blood capillaries in being covered by a single layer of endothelial cells. However, they are 100 500 times more permeable with fenestrations or pores having a size of 50 100 nm.
Malpighian Body (Ronal Corpuscle): The complex formed by the glomerulus, connective tissue, and Bowman’s capsule is called the Malpighian body or renal corpuscle.
Proximal Convoluted Tubule (PCT): The lower part of Bowman’s capsule leads into the proximal convoluted tubule.
- The latter is present in the cortex
- It is twisted and surrounded by peritubular blood capillaries.
- PCT is lined by cuboidal epithelium having brush borders with long microvilli for increasing absorptive area.
- The cells contain abundant mitochondria and food reserves for providing energy to perform active absorption and secretion.
Loop of Henle: The loop of Henle is a hairpin loop-like tubular part of the nephron that descends into the renal medulla.
- It is made of two parallel limbs joined by a curved base.
- There is a descending limb and an ascending limb.
Descending limb: The descending limb is in continuation with the proximal convoluted tubule and has two parts—a thick segment and a thin segment.
- The thick segment constitutes about four-fifths of the descending limb.
- It lies inside both the cortex and medulla.
- The cells lining it are cuboidal.
- They have sparse microvilli and fewer mitochondria indicating that active absorption and secretion are absent.
- A thin segment is the narrow part of the descending limb.
- It lies in the medulla and is lined by flat epithelial cells having sparse microvilli and few
mitochondria. - The thin segment gets curved to become a part of the ascending limb.
Ascending limb: Ascending limb consists of a thin segment in the proximal part and a thick segment afterward.
- The thin segment is lined by flat epithelial cells which allow passive diffusion of some solutes (e.g., Na+, Cl– ) depending upon their concentration gradient.
- The thick segment of the ascending limb is wider and lined by cuboidal cells having microvilli as well as mitochondria.
- The thick ascending segment is involved in the active secretion of NaCl in the medulla.
Vasa Recta: The loop of Henle is covered by a staircase of blood capillary network arising from efferent glomerular arteriole called vasa recta. It forms a counter-current system with the loop of Henle having an ascending branch in the area of the descending limb and a descending branch in the area of the ascending limb.
Distal Convoluted Tubule (DCT): The distal convoluted tubule is a highly coiled part of the nephron and lies close to the Malpighian body.
- The epithelial lining of the distal convoluted tubule consists of cuboidal cells having sparse microvilli and deep mitochondria.
- The distal convoluted tubule is covered by peritubular blood capillaries.
- The last part of the distal nephron is nearly straight, called the connecting or junctional tubule, and opens into a collecting duct.
Collecting ducts: Each nephron opens into a wider collecting tubule in the area of the cortex.
- Collecting tubules are lined by specialized cuboidal epithelium with very few microvilli.
- They open into still wider collecting ducts.
- Collecting ducts enter the medulla and form ducts of Bellini.
- The ducts run through renal pyramids.
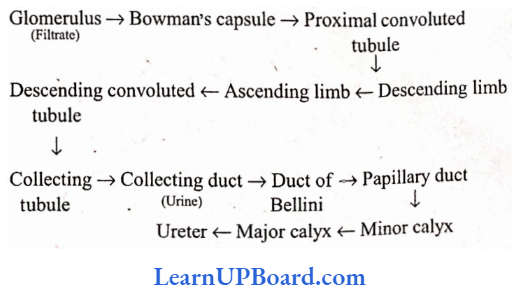
Route Of Urine Flow:
NEET Biology Notes Excretory Products And Their Elimination Physiology Of Excretion (Mechanism Of Urine Formation)
Nephric excretion involves the formation of urine. Urine formation occurs in three steps—glomerular filtration, tubular reabsorption, and tubular secretion.
Glomerular Filtration (Ultrafiltration): Blood present in the glomerular capillaries is separated from the capsular space of Bowman’s capsule by
- The endothelial covering of blood vessels
- The basement membrane of blood vessel
- The basement membrane of the visceral layer
- The visceral layer or inner wall of Bowman’s capsule
Therefore, the actual barrier between blood and capsular space consists of two basement membranes which are, however, permeable to small-sized molecules.
Development of filtration pressure: Blood flows through glomerular capillaries under pressure. The pressure is due to two reasons:
- The wider diameter of the afferent arteriole as compared to the diameter of the efferent arteriole.
- Natural arterial pressure is caused by the pumping activity of the heart. Blood pressure in glomerular blood is about 60 mm Hg. This is called glomerular hydrostatic pressure (GHP). The osmotic concentration of the proteinaceous content of glomerular blood is equivalent to 30 mm Hg. This is called blood colloidal osmotic pressure (BCOP).
- The pressure of interstitial fluid and the pressure of renal filtrate is collectively called capsular hydrostatic pressure (CHP = 20 mm Hg). The pressure being exerted on glomerular blood for undergoing filtration is called glomerular filtration pressure (GFP). It is about 10 mm Hg.
or, GFP=GHP-(BCO+CHP)
=60-(30+20)=10mm Hg
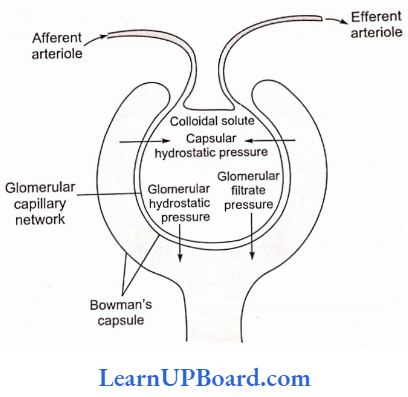
Ultrafiltration: As there is a net higher hydrostatic pressure of 10 mm Hg in the lumen of glomerular capillaries as compared to the lumen of Bowman’s capsule, the filterable components of blood are passed out of the glomerular capillaries.
- The blood components pass through endothelial fenestrations, basement membranes, and filtration slits of podocytes to enter the lumen of Bowman’s capsule.
- The phenomenon is called nephric or glomerular filtration.
- About 1100-1200 mL of blood is put to filtration in the two kidneys every minute which constitutes roughly one-fifth of the blood pumped out by each ventricle of the heart in a minute.
- It produces a glomerular or nephric filtrate of about 125 mL/min or 180 L/day.
- The rate of filtration is called glomerular filtration rate (GFR).
- Nephric filtrate consists of water, various electrolytes (Na+, K+, Ca2+, Mg2+, K+, PO43-), glucose, amino acids, hormones, vitamins, urea, creatinine, uric acid, etc. It is alkaline like blood but excludes large-sized particles and structures such as fats, proteins, platelets, leucocytes, and erythrocytes.
- The separation of small-volume solutes from large-volume solutes and components due to filtration through small-sized pores or slits by the application of pressure is called ultrafiltration.
Autoregulation of glomerular filtration: There are three methods by which renal blood flow and GFR are automatically regulated.
- Myogenic Autoregulation
- A rise in blood pressure should normally increase blood flow through glomeruli.
- However, stretching of the vascular wall increases the passage of Ca2+ ions from extracellular fluid into the cells resulting in their contraction.
- Contraction checks overstretching of the vascular walls and raises vascular resistance so that the rate of blood flow and GFR are brought down to normal.
- Juxtaglomerular apparatus (JGA)
- The apparatus becomes active when there is a decrease in renal blood pressure or a decrease in GFR.
- It promotes the release of renin from juxtaglomerular cells.
- Renin converts protein angiotensinogen into peptide angiotensin.
- Angiotensin is a hormone that raises glomerular blood pressure through constricting efferent arterioles resulting in restoring GFR.
- It also brings about the release of aldosterone.
- Neural control
- Blood vessels of the kidney are innervated by nerve fibers of the sympathetic nervous system.
- When activated, the nerve fibers bring about constriction of renal arteries and cause a decrease in the renal blood flow as well as GFR.
Tubular Reabsorption
- Ultrafiltration is non-selective. Therefore, the glomerular filtrate contains both waste products as well as useful essential solutes.
- The absorption of useful essential substances from the glomerular filtrate by the epithelium of uriniferous tubules for transfer to interstitial fluid and peritubular capillaries is called reabsorption.
- Reabsorption occurs by both active and passive processes.
- Active reabsorption occurs against a concentration gradient. It requires energy. Because of this, kidneys consume more oxygen than even the heart.
- Passive absorption does not require energy. It occurs along a concentration gradient.
- Reabsorption occurs in all parts of the uriniferous tubule—proximal convoluted tubule, a loop of Henle, distal convoluted tubule, collecting tubule.
Reabsorption In Proximal Convoluted Tubule: PCT is the major seat of reabsorption.
- For this, its epithelial cells possess abundant mitochondria and microvilli.
- Microvilli increase the absorptive surface by some 20 times.
- More than two-thirds volume of glomerular filtrate (essential nutrients 70-80% of electrolytes and water) is reabsorbed in the proximal convoluted tubule.
- It includes the whole of glucose, most of Ca2+, amino acids, ascorbic acid, 75% K+, 70% Na+, 75% water, 90% HCO3–, and a good quantity of CF and some other anions.
- Reabsorption of Na+, K+, and Ca2+ occurs through active transport.
- Glucose and amino acids are reabsorbed through secondary active transport.
- Cl– and other anions are reabsorbed through diffusion.
- Water passes out due to osmosis which is also a process of diffusion.
- The filtrate, however, remains isotonic to blood.
class 11 biology chapter 19 notes pdf
Reabsorption in the loop of Henle: The loop of Henle is the seat of further concentration of pre-urine though tonicity is not much influenced.
Descending limb: The thick segment is nearly impermeable.
The thin segment which lies in the hypertonic interstitial fluid of the medulla loses a lot of water due to osmosis. It makes the filtrate hypertonic. Therefore, the descending limb is also called the concentrating segment.
Ascending Limb: The ascending limb is impermeable to water.
- The thin segment loses NaCl to interstitial fluid through diffusion.
- The thick segment actively transports NaCl into the outer interstitial fluid.
- This contributes to the high osmolarity of the inner medulla of the kidney.
- Some transport also occurs of Mg2+, Ca2+, and K+. Due to the loss of NaCl, the filtrate becomes hypotonic to blood plasma in the ascending limb of the loop of Henle. Because of this, the ascending limb of the loop of Henle is also called the diluting segment.
Reabsorption in distal convoluted tubule: It depends upon the activity of hormones aldosterone and vasopressin. Under the influence of aldosterone, Na+ is actively reabsorbed from the filtrate. Cl– accompanies it passively. HCO3– also passes out. Vasopressin or ADH, if available, helps in the reabsorption of water.
Reabsorption in collecting tubules and collecting ducts: Their walls become permeable and allow reabsorption of water only if the hormone vasopressin or ADH (anti-diuretic hormone) is available. In the presence of the hormone, water passes out from the filtrate and the urine becomes more and more hypertonic as the ducts dip in the medulla. In the absence of the hormone, dilute hypotonic urine passes out. A part of the urea diffuses out of the bottom parts of collecting ducts into the medulla part. It makes the medulla hyperosmotic.
Tubular Secretion
As only 15-25% of blood plasma is filtered out of glomerular filtrate, a lot of waste products remain in the arteriolar blood present in peritubular capillaries around the nephric tubules. These wastes are actively secreted into the nephric filtrate in PCT and OCT.
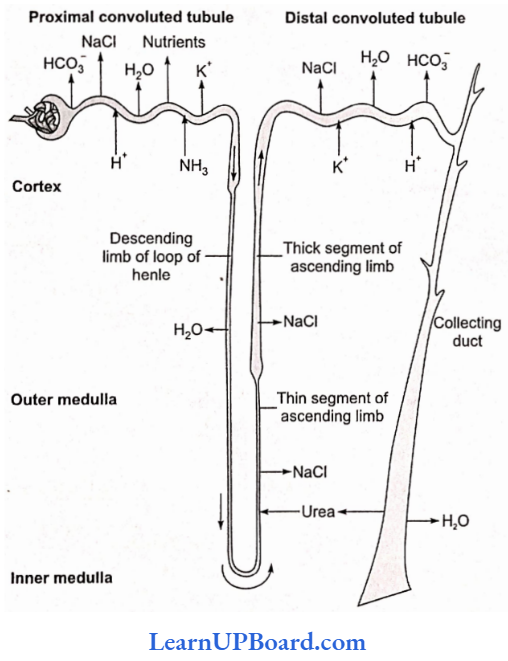
NEET Biology Notes Excretory Products And Their Elimination Counter Current Mechanism
The concentration of urine is due to the loop of Henle. The capability of concentrating the urine is largely related to the length of the loop of Henle.
- Concentration is also helped by the vasa recta and the flow of urea.
- The loop of Henle and vasa recta, both form counter counter-current system, which is significantly involved in concentrating the urine.
- The descending limb of the loop of Henle is permeable to water.
- The osmolarity of the filtrate as it is formed is about 300 mm/L.
- As the filtrate moves from the cortex to the inner medulla, the osmolarity increases to 1200 mosm/L as the water passes out of the filtrate.
- Two solutes which contribute to the gradient of osmolarity are NaCI and urea.
- As the concentrated filtrate enters the ascending limb, NaCI leaks out from the thin segment of the ascending limb.
- Additional salt is actively transported out of the thick limb of the ascending limb.
- The filtrate makes a total of three trips between the cortex and medulla: first down the descending limb, up the ascending limb, and down the collecting duct.
- NaCI is transported by the ascending limb of Henle’s loop which is exchanged with the descending branch of vasa recta.
- NaCI is returned to the interstitium by the ascending portion of the vasa recta. Similarly, a small amount of urea enters the thin segment of the ascending limb of Henle’s loop which is transported back to the interstitium by the collecting duct. This transport of substances facilitated by the special arrangement of Henle’s loop and vasa recta is called the counter-current mechanism.
- This helps in maintaining a concentration gradient in the medullary interstitium, which helps in an easy passage of H, from the collecting duct, thereby concentrating the filtrate (urine).
- Human kidneys can produce urine in nearly four times more concentrated filtrate than the initial filtrate formed.
NEET Biology Notes Excretory Products And Their Elimination Regulation Of Kidney Function
Control By Antidiuretic Hormone
- Antidiuretic hormone (ADH) is produced in the hypothalamus of the brain and released into the bloodstream from the pituitary gland. It enhances fluid retention by making the kidneys reabsorb more water.
- The release of ADH is triggered when osmoreceptors in the hypothalamus detect an increase in the osmolarity of the blood above a set point of 300 mm/L. In this situation, the osmoreceptor cells also promote thirst.
Drinking reduces the osmolarity of the blood, which inhibits the secretion of ADH, thereby completing the feedback circuit.
Control By Juxtaglomerular Apparatus: Juxtamcdullary nephrons help in retaining Naf ions in high concentration in the interstitial fluid between the nephrons.
- The juxtaglomerular apparatus operates a multi-hormonal renin-angiotensin-aldosterone system (RAAS).
- The JGA responds to a decrease in the blood pressure or blood volume in the afferent arteriole of the glomerulus and releases an enzyme, renin, into the bloodstream. Renin initiates chemical reactions that convert a plasma protein called angiotensinogen to a peptide called angiotensin which works as a hormone.
- Angiotensin is a powerful constrictor of arterioles, one of the most potent vasopressor substances known.
- Angiotensin increases blood pressure by causing arterioles to constrict.
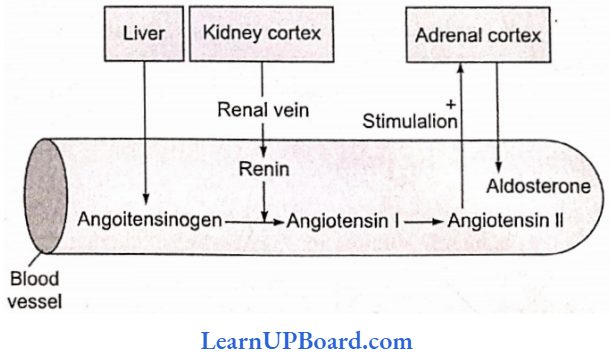
- Angiotensin also increases blood volume in two ways: firstly, by signaling the proximal convoluted tubules to reabsorb more NaCI and water, and secondly, by stimulating the adrenal gland to release aldosterone, a hormone that induces the distal convoluted tubule to reabsorb more Na+ and water.
- This leads to an increase in the blood volume and pressure, completing the feedback circuit by supporting the release of renin.
- Atrial natriuretic factor (ANF) opposes the regulation by RAAS.
- The wall of the atria of the heart releases ANF in response to an increase in blood volume and pressure.
- ANF inhibits the release of renin from JGA. This inhibits the reabsorption of Na+ by the collecting duct and reduces the release of aldosterone from the adrenal gland.
- It also increases the excretion of Na+ in urine.
Micturition: The voiding or expulsion of urine stored in the urinary bladder is called micturition.
- The urinary bladder gets gradually filled up with urine.
- Though the capacity urinary bladder is above 800 mL, as the volume reaches around 500 mL, the bladder wall starts getting stretched.
- The urine formed by nephrons is ultimately carried to the urinary bladder where it is stored till a voluntary signal, which is initiated by the stretching of the urinary bladder as it gets filled with urine.
- Stretch receptors generate nerve impulses that are carried by sensory neurons to the brain producing the sensation of fullness. This initiates the autonomic reflex (parasympathetic involving sacral spinal nerves) resulting in the contraction of detrusor muscles of the urinary bladder and inhibition of motor impulse of the voluntary, striated external sphincter, making it relaxed; and urine comes out.
- Micturition can be initiated voluntarily also by contracting the abdominal muscle which applies pressure over the urinary bladder, activating the stretch receptors.
NEET Biology Notes Excretory Products And Their Elimination Composition Of Urine
An adult human excretes an average of 1-1.5 L of urine per day. Urine is mainly composed of water (96%) and urea (2%). Other dissolved solids (2%) are as follows:
- Uric acid—derived from nucleic acid metabolism (purine)
- Creatinine—an organic byproduct of muscle metabolism
- Inorganic salts—chlorides, phosphates, sulfates, and oxalates of Na, K, and Ca. Small quantities of NH3, urobilin, and hematoporphyrin are also present.
Urine could be transparent or pale yellow (due to urochrome, a breakdown product of hemoglobin). It is acidic (pH = 6.0) but differs depending on dietary intake. Intake of more fruits and proteins in the diet makes it acidic while intake of vegetables increases alkalinity. The unpleasant or ammonical smell of urine is due to the conversion of urea into ammonia by microbial action.
Abnormal Constituents in Urine: Sometimes, urine may be diagnosed with some unusual constituents mentioned below.
- Protein (albumin): During injury to the renal tract—glomerulonephritis
- Bile salts: During jaundice
- Glucose: During diabetes mellitus
- Ketone bodies (acetoacetic acid, (3-hydroxybutyric acid): During diabetes mellitus, prolonged fasting.
- Creatinine: Hyperthyroidism, starvation
NEET Biology Notes Excretory Products And Their Elimination Diseases Of Urinary Tract
Nephritis: The infection is caused by bacteria which results in kidney inflammation.
- Glomerulonephritis: Inflammation of glomeruli.
- Pyelonephritis: Inflammation of kidney tissues in the pelvis region,
- Cystitis: Inflammation of the urinary bladder.
- Renal calculi: Stone or insoluble mass of crystallized salts (oxalate, etc.) formed within the kidney.
- Polyurea: The amount of urine passed out is more.
- Uremia: Increased concentration of urea in blood.
- Alkaptonuria: It is a genetic disease in which homogentisic acid is excreted out with urine.
- Pyuria: Presence of pus in the urine.
- Glycosuria: Presence of glucose in urine.
- Hematuria: Presence of blood in the urine.
- Inulin: It is a fructan (storage polysaccharide). It cannot be metabolized in the human body and is readily filtered through the kidneys. It is, therefore, used in testing kidney function, especially GFR.
- Tubular maxima: The maximum amount of substance that can be retained in the blood and beyond which it will be excreted in the urine.
NEET Biology Notes Excretory Products And Their Elimination Artificial Kidney
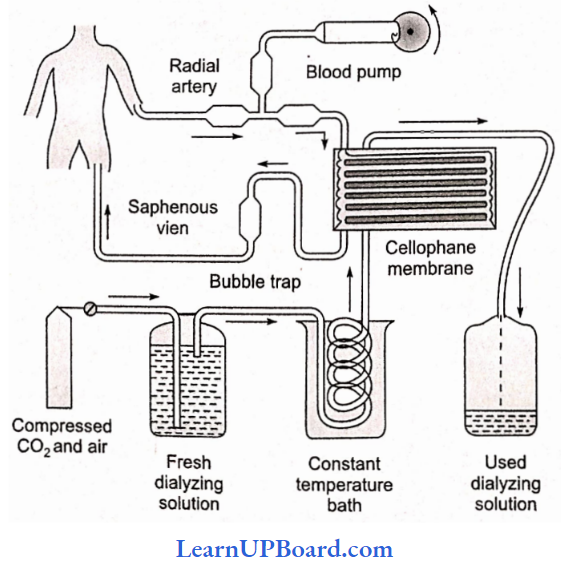
When kidneys are completely damaged and do not function, the patient often receives hemodialysis (treatment with an artificial kidney).
- Hemodialysis is the separation of certain substances from blood by use of a selectively permeable membrane.
- The pores in the membrane allow some substances to pass through; however, they prevent others.
- The patient is connected to the machine by a tube attached to an artery, often the radial artery.
- Blood from the artery is pumped into a tube that runs through the dialyzer.
- The dialyzer is filled with dialysis fluid which contains the same quantities of electrolytes and nutrients as normal plasma but contains no waste products.
- A cellophane tube (a tube bounded by a thin membrane) is kept in the dialysis fluid.
- The pores in the cellophane tube do not allow movement of the blood cells and proteins from the blood into the dialysis fluid but are large enough to allow smaller molecules to diffuse into the fluid.
- Molecules of waste substances such as urea, ammonia, etc., diffuse into the dialysis fluid.
- Diffusion of other substances such as glucose, amino acids, and electrolysis is prevented by the presence of these substances in the dialysis fluid in the same concentration as in the normal plasma.
- Now the blood is returned to the patient’s body through a vein, usually the radial vein.
- When the blood is taken out, it is cooled to 0°C, mixed with an anticoagulant, and then pumped into an artificial kidney.
- The blood coming out of the artificial kidney is warmed up to body temperature, is mixed with anti-heparin, and returns to a vein.
Kidney Transplantation: When both kidneys are completely damaged, kidney transplantation is done.
- The world’s first successful organ transplant was kidney transplantation which was undertaken by David Hume and Joseph Kelly at Peter Bent Brigham Hospital in Boston in 1954.
- The recipient was Richard Herrick who lived further for eight years. The first kidney transplant in India was performed on December 1, 1971, at Christian Medical College, Vellore (Tamil Nadu), on a 35-year-old patient named Shanmughan.
- Most patients need to be dialyzed before transplantation to avoid fluid overload and hyperkalemia after the operation.
- Antibiotics and immunosuppressive drugs are given before the operation.
- Postoperative care is very essential.
NEET Biology Notes Excretory Products And Their Elimination Accessory Excretory Organs In Man
Lungs: Lungs help in removing CO2 and water. They eliminate around 18 L of CO2 per hour and about 400 mL of water per day in normal resting conditions.
The water loss will increase in cold dry climatic conditions and will decrease in hot, humid climates. Different volatile materials are also readily eliminated through the lungs.
Skin: The skin contains a large number of sweat glands richly supplied with blood capillaries, from which they excrete sweat and some metabolic wastes.
- Since skin sends out plenty of water and a small amount of salts, hence it serves as an excretory organ.
- Sebaceous glands in the skin eliminate sebum which contains waxes, sterols, some hydrocarbons, and fatty acids.
Liver: It produces bile pigments which are metabolic wastes of hemoglobin of dead RBCs.
The liver is also the main site for the elimination of cholesterol, inactivated products of steroid hormones, some vitamins, and many drugs.
Large intestine: Epithelial cells of the large intestine excrete Ca2+, Mg2+, and Fe2+ into the lumen of the intestine which comes out along with fecal matter.
NEET Biology Notes Excretory Products And Their Elimination Assertion-Reasoning Questions And Answers
In the following questions, an Assertion (A) is followed by a corresponding Reason (R). Mark the correct answer.
- If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
- If both Assertion and Reason are true, but the Reason is not the correct explanation of the
Assertion. - If Assertion is true, but Reason is false.
- If both Assertion and Reason are false.
Question 1.
Assertion: Pregnant women may show some presence of glucose in their postprandial urine although they have no diabetes.
Reason: In pregnant women, the glomerular filtration rate is slightly increased. As a result the
tubular load of glucose exceeds the tubular maximum for glucose reabsorption.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 2.
Assertion: The atrial natriuretic factor is released by a wall of atria.
Reason: It inhibits the release of renin from the juxtaglomerular apparatus.
Answer: 2. If both Assertion and Reason are true, but the Reason is not the correct explanation of the Assertion.
Question 3.
Assertion: The inner wall of Bowman’s capsule is lined with specialized cells “podocytes” having a number of projections.
Reason: These projections increase the surface area for absorptions.
Answer: 3. If Assertion is true, but Reason is false.
Question 4.
Assertion: Kidneys are retroperitoneal in position.
Reason: Kidneys are covered with peritoneum only on the ventral surface.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 5.
Assertion: Uric acid is produced by the metabolism of purine and pyrimidine.
Reason: Uric acid has high toxicity and is soluble in water.
Answer: 4. If both Assertion and Reason are false.
Question 6.
Assertion: Kidneys of the vertebrates are retroperitoneal and extra-coelomic.
Reason: The structural and functional units of the kidneys are nephrons.
Answer: 2. If both Assertion and Reason are true, but the Reason is not the correct explanation of the Assertion.
Question 7.
Assertion: The glomerular filtrate resembles the protein-free plasma in composition and osmotic pressure.
Reason: The glomerular capillary wall and inner membrane of Bowman’s capsule are impermeable to large molecules.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 8.
Assertion: During micturition, urine is prevented from flowing back into the ureters.
Reason: Urethral sphincters relax during micturition.
Answer: 2. If both Assertion and Reason are true, but the Reason is not the correct explanation of the Assertion.
Question 9.
Assertion: Kidneys maintain the osmotic concentration of the blood.
Reason: Kidneys eliminate either hypotonic or hypertonic urine according to the body’s needs.
Answer: 1. If both Assertion and Reason are true and the Reason is the correct explanation of the Assertion.
Question 10.
Assertion: ADH reduces chloride loss in urine.
Reason: ADH decreases water absorption.
Answer: 4. If both Assertion and Reason are false.
