UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Learning Objectives
After completing this chapter, you will be able to:
- Define excretion and mention its importance;
- Describe the nature of excretory wastes produced in our body,
- Identify different parts of the excretory system and describe their functions; Excretion – Elimination of Body Wastes
- Describe the gross anatomy of the kidney,
- Identify the parts of the nephron responsible for urine formation;
- Explain the physiology of urine formation; describe the mechanism of osmoregulation by the kidney.
Various waste products are formed in our bodies continuously as a result of many metabolic activities taking place inside the body. These waste substances, if accumulated, would poison cells or slow down metabolism. Hence, the body must get rid of these unwanted substances. The metabolic wastes to be excreted include CO₂, H₂O, fats, ammonia, urea, uric acid, etc.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Excretion-Elimination of Body Wastes Excretion
- The removal of waste products formed in the body as a result of metabolism is termed excretion. Excretion can also be defined as the removal of mainly nitrogenous wastes from the body. The lungs and kidneys are the main organs of excretion in human beings. The process of maintaining the right amount of water and proper ionic balance in the body is called osmoregulation.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Nature Of Excretory Wastes
- The wastes formed as a result of various metabolic activities are:
1. Respiratory waste formed as a result of oxidation of glucose (food) (through cellular respiration):
- These mainly constitute carbon dioxide and water.
- The carbon dioxide is eliminated from the body through the lungs (during expiration).
- Water becomes a part of the rest of the water contained in the body.
2. Nitrogenous waste formed as a result of deamination of unwanted amino acids, body’s own proteins and nucleic acids: The three main nitrogenous waste products excreted by animals are ammonia, urea and uric acid. Urea is a highly poisonous waste product and its accumulation beyond a certain concentration in the body may cause death. Urea is eliminated through the kidneys.
| Class 10 Science | Class 11 Chemistry |
| Class 11 Chemistry | Transformation of Sentences |
| Class 8 Maths | Class 8 Science |
3. Other waste like salts (NaCl), excess vitamins and water, which we take directly through food: Excess salts are mainly excreted by kidneys.
4. The excess water is removed by kidneys as urine and some of it is excreted as sweat by the sweat glands on our skin.
5. Bile pigments are formed due to the breakdown of haemoglobin in dead RBCs in the liver. A large amount of these pigments is excreted out in faeces while some of it is excreted in the urine.
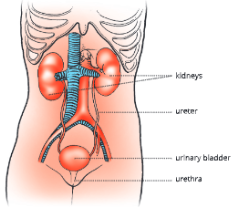
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Human Urinary System
The urinary system in human beings consists of the following parts.
- A pair of kidneys
- A pair of ureters
- Urinary bladder
- Urethra
1. Kidneys
- The kidneys are reddish-brown, paired structures located on either side of the vertebral column (backbone). They are protected by the last two pairs of ribs. Kidneys in human beings are said to be retroperitoneal because they lie behind the peritoneal lining of the abdominal cavity.
- Each kidney is a bean-shaped organ, about 10 cm long, 6 cm wide and 4 cm thick. The right kidney is positioned slightly at a lower level than the left kidney as the right side of the abdominal cavity is occupied by the liver. They are held in position by a padding. On the inner concave side of the kidney, a notch called the hilum is present. It is the place from where the ureter and the renal vein come out and the renal artery enters the kidney.
2. Ureters
- The ureters arise from within the renal sinus of the kidney at hilum. The front end of each ureter is extended into a funnel-shaped structure, the renal pelvis. The ureters transport urine from the kidneys to the urinary bladder. Each ureter opens obliquely in the urinary bladder by a slit-like aperture to prevent the backflow of the urine.
3. Urinary bladder
- The urinary bladder is a muscular reservoir for storage of urine. It lies in the pelvic cavity of the abdomen. The neck of the urinary bladder is surrounded by sphincters. Sphincter acts like a valve which remain closed until the time of micturition (urination) described below.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Role Of The Urinary Bladder In Urination
- Besides functioning as a temporary reservoir of urine, the bladder also evacuates the urine at suitable intervals. The act of voiding or discharging urine is called micturition.
- When enough urine gets accumulated in the bladder to raise its pressure sufficiently, a spontaneous nervous activity (reflex) is initiated. This causes the smooth muscles on the bladder wall to contract and the urethral sphincter to relax. Urine flows to the outside. As the ureters enter obliquely through the bladder wall, their openings get shut due to compression by the contracting bladder muscles and backward flow of urine is prevented.
4. Urethra
- The urethra is a tube that arises from the neck of urinary bladder and extends up to the outside. In males, it serves as a common passage for urine and sperm. The urethra in females serves as a passage for urine only.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Internal Structure Of The Kidney
- Each kidney in a longitudinal section shows two distinct regions- an outer renal cortex and an inner renal medulla. The medulla is subdivided into 15 or 16 conical masses, the renal pyramids. Due to presence of these pyramids, the medulla has a striped appearance.
- Each pyramid has a narrow renal papilla toward the pelvis and a broad base toward the cortex. Renal papillae open into a wide funnel-like structure, renal pelvis. The renal pelvis in turn leads into the ureter.
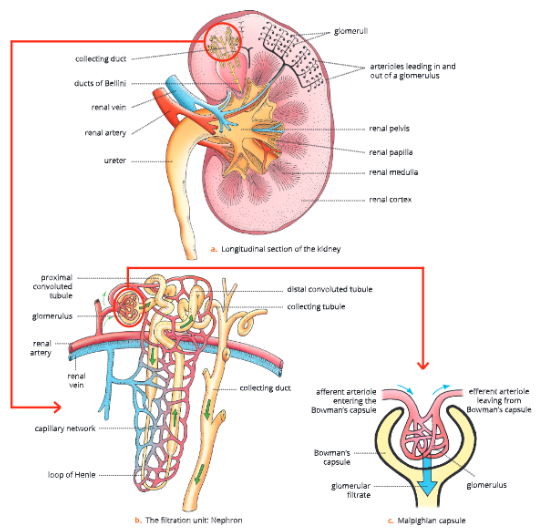
Nephron – structural and functional unit of kidney
- Each kidney consists of more than one million nephrons or uriniferous tubules. Nephron is the functional unit of a kidney. Each nephron consists of – a Malpighian capsule, a nephric tubule (secretory part of uriniferous tubule) and a collecting tubule.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Structure Of Malpighian Capsule
- It has two parts a Bowman’s capsule and a glomerulus.
- Bowman’s capsule: It forms the dilated blind end of the nephron. It is a double-walled, cup-shaped structure. It is lined by a thin semipermeable squamous epithelium. The outer concavity of Bowman’s cup contains a knot-like mass of blood capillaries called glomerulus.
- Glomerulus: The afferent arteriole enters the Bowman’s capsule and divides into a bunch of about 50 capillaries. This bunch is called glomerulus. Their diameter gets reduced to increase the blood pressure. Bowman’s capsule together with the glomerulus are called renal capsule or Malpighian capsule.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Nephric Or Uriniferous tubule
- It is a long, coiled tubule and can be divided into three major -regions the proximal convoluted tubule (PCT), the loop of Henle and the distal convoluted tubule (DCT).
- Proximal convoluted tubule (PCT): It is the initial (proximal) convoluted region of the nephric tubule nearer to the Bowman’s capsule. It is a highly coiled structure and is about 12-24 mm in length. It is lined by the columnar epithelium and is provided with microvilli. PCT is located in the cortex region of kidney.
- Loop of Henle: It is a U-shaped loop formed in the middle of the nephric tubule. It has a thin descending limb and a thick ascending limb. The descending limb is lined with flattened epithelial cells, while the ascending limb is lined with cuboidal epithelium. It is not convoluted. It runs in the medulla and turns back to cortex region.
- Distal convoluted tubule (DCT): It is a convoluted structure and is present in the cortex region. It is lined by cuboidal epithelium. It opens into the collecting tubule.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Collecting Ducts And The Ducts Of Bellini
- Collecting ducts are larger ducts, each receiving collecting tubules from nephrons. These pass into the renal medulla and join with each other forming still larger ducts of Bellini. These ducts drain the urine collected from the nephrons into the renal pelvis which leads to the ureter.
Blood Supply To Kidney Tubules
- Each kidney receives blood supply from renal arteries branching off from dorsal aorta. These arteries further branch off into arterioles and each arteriole, called afferent arteriole, enters inside Bowman’s capsule.
- It branches further and forms a mass of capillaries called glomerulus. The fine capillaries of glomerulus reunite and form efferent arteriole. Efferent arteriole comes out of Bowman’s capsule and surrounds renal tubule. They further rejoin and form renal veins which kidney and empty into posterior vena cava.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Physiology Of Urine Formation
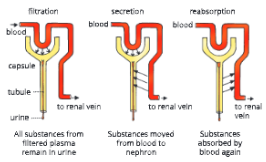
- Urine formation involves three main processes – ultrafiltration, tubular reabsorption and tubular secretion.
1. Ultrafiltration
- Walls of glomerular capillaries and Bowman’s capsule are very thin and semipermeable in nature. Hence, they act as ultrafilters.
- The glomerular hydrostatic pressure or the capillary pressure is the main driving force that tends to move fluid out of the glomeruli. It is exerted by the blood while passing through the glomerulus.
Why is hydrostatic pressure more in glomerulus?
Hydrostatic pressure is more in glomerulus because
- The afferent arteriole entering the Bowman’s capsule is wider than the efferent arteriole leaving it. As a result, more blood enters the glomerulus while less blood moves out. This is the reason behind the high hydrostatic pressure in the glomerulus.
- Due to this high filtration pressure in the blood of glomerulus, a part of water and dissolved constituents of blood (like nitrogenous wastes, glucose, amino acids, mineral ions, etc.), are filtered out in the Bowman’s capsule. This forms the glomerular filtrate. Filtration under high pressure is called ultrafiltration.
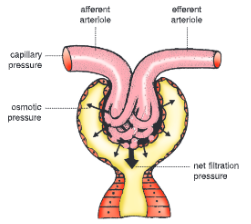
- During ultrafiltration, nearly all the liquid components of blood come out of glomerulus and pass into the funnel of Bowman’s capsule. The rest of the blood, left behind in the glomerulus after ultrafiltration is very thick (because the liquid part has been removed) and is carried forward by the efferent arteriole.
- The glomerular filtration rate in adults is 120 mL per minute and the filtrate produced daily amounts to about 172 litres.
2. Tubular reabsorption or selective reabsorption
- Our body cannot afford to lose several useful substances that are filtered in the glomerular filtrate. As this filtrate flows through the nephric tubule, water and several useful substances (solutes) are reabsorbed through the wall of the renal tubule (nephric tubule) and returned to the blood flowing in peritubular capillaries. This is called selective reabsorption.
- Water is reabsorbed by osmosis. Selective reabsorption of glucose, amino acids and salts also take place.
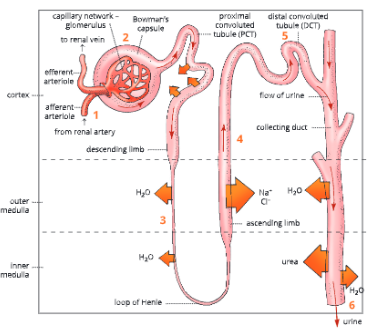
- In the PCT, 65-80 per cent of the filtrate is reabsorbed. It includes water, glucose, amino acids and minerals like Na+, K+ and Ca++.
- In the descending limb, 5 per cent water is reabsorbed.
- In the ascending limb, only minerals (Na+, K+, Cl-) are reabsorbed. The ascending limb is impermeable to water.
- In the DCT and collecting ducts, Nat is reabsorbed under the influence of hormone aldosterone and water is reabsorbed under the influence of hormone ADH (antidiuretic hormone).
3. Tubular secretion
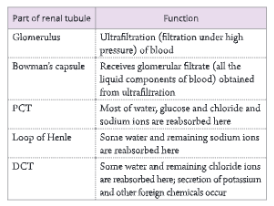
- This process is the converse of tubular reabsorption. The cells of the renal tubule also remove wastes from blood and pass into the filtrate by the process of secretion. Tubular secretion removes ammonia, urea, uric acid, creatinine and hippuric acid from the blood. The function of various parts of renal tubule in formation of urine are given in Table.
- Blood from renal artery enters kidneys.
- Ultrafiltration: Blood enters glomerular capillaries. Water and small solutes are filtered in Bowman’s capsule.
- Tubular reabsorption: Water and many solutes are reabsorbed through the wall of nephric tubule and return to the blood in peritubular capillaries.
- Tubular secretion: Cells of renal tubule remove wastes from blood and pass them into filtrate.
- Hormonal action adjusts the urine. concentration. ADH promotes water reabsorption. Aldosterone influences reabsorption of sodium and potassium.
- Urination: Water and solutes flow to renal pelvis, then eliminated out through urinary tract.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Hormonal Control Of Urine Formation
- Urine formation is under the control of two hormones – antidiuretic hormone (ADH) and aldosterone.
- Antidiuretic hormone (ADH) or vasopressin released from the posterior lobe of pituitary gland, increases the permeability of the renal tubule to water. When the blood plasma is concentrated, more ADH is secreted and more water is reabsorbed in the urinary tubules. Hence, urine passed out from body is concentrated, for example in summer. When the blood plasma is diluted, less ADH is secreted and less water is reabsorbed in the urinary tubule. In this case, a large amount of dilute urine is passed out of the body, for example in winter.
- Aldosterone, a hormone released from the adrenal cortex, influences reabsorption of sodium and potassium. This hormone regulates the amount of sodium and potassium that is to be retained in the blood and is to be excreted.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Urine And Its Composition
- An adult man normally passes about 1-1.5 litres of urine in a day. Urine is a transparent yellowish fluid. Its yellow colour is due to a pigment urochrome derived from the breakdown of haemoglobin of worn-out RBCs,
- Its pH range is 5-8. It has an unpleasant odour. If allowed to stand, the urea present in urine is degraded by bacteria to ammonia, which gives a strong awful smell to it.
- In normal composition, urine consists of 95 per cent water, and rest 5 per cent is the organic and inorganic substances (solid wastes). Each litre of urine contains nitrogenous organic compounds – urea 2.3 g, uric acid 0.7 g, creatinine 1.5 g and a negligible amount of hippuric acid. Of these, urea is the principal nitrogenous waste in human urine. The non-nitrogenous organic compounds include vitamin C, oxalic acid and phenolic substances.
- The inorganic substances include ammonia (0.6 g/L) and mineral salts, such as phosphates, sulphates and chlorides of Na, K, Ca and Mg. Sodium chloride (9.0 g/L) is the principal mineral salt in the urine.
- Abnormal components of urine include albumin, bile salts, bile pigments, glucose and ketone bodies, which occur in the urine in various pathological conditions.
Common diseases related to abnormal composition of urine
- Glycosuria: Urine with high glucose due to diabetes mellitus
- Albuminuria: Urine with albumin due to high blood pressure
- Ketonuria: Urine with ketone body
- Jaundice/Hepatitis/Liver cirrhosis: Urine with bile pigment
- Pyuria: Urine with pus cells
- Haematuria: Urine with blood cells due to urinary tract infection or kidney stone
- Diabetes insipidus: Urine with excess of water (frequent passing out of large quantities of urine) due to deficiency of ADH or vasopressin
Role ADH and insulin in urine
- The hormone vasopressin or antidiuretic hormone (ADH) regulates the output of urine. This hormone is secreted by the posterior lobe of the pituitary gland. When the secretion of this hormone gets reduced, the amount of urine produced is increased, causing diabetes insipidus disorder. Sometimes hyposecretion of the insulin hormone causes diabetes mellitus disease in which excess glucose is passed with urine.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Osmoregulation By The Kidney
- The water and solute content of body fluids is regulated by the kidney. This function of the regulation of osmotic concentration of the blood by the kidney is called osmoregulation.
- In human beings, the kidney is extremely flexible in its working. Generally, in summer when most of water is lost from the body by perspiration, the urine passed out is hypertonic.
- However, in winter as there is no perspiration, the urine passed out is hypotonic. This flexibility in the working of human kidney and renal tubules is brought about by the movement of water and Na+ in and out of nephron under the influence of certain hormones, thus osmolarity is regulated.
When there is excess of water in body fluids
In such a condition, the urine passed out of the body is more dilute (hypotonic) than the body fluids. It is achieved by two processes:
- Excess of water increases blood volume which increases the hydrostatic pressure in glomerulus, hence, more nephric or glomerular filtrates are formed.
- The sensation of excess of water in the body fluid is received by osmoregulator cells in the hypothalamus part of the brain.
- These cells in turn influence the posterior lobe of the pituitary gland to inhibit or reduce the release of antidiuretic hormone (ADH). A deficiency of ADH reduces the permeability of cells in the distal convoluted tubule and collecting duct, thereby decreasing the real notion of water.
- More filtration and less reabsorption of water produce excessively dilute urine. This brings down the volume of the body fluids to normal.
If the body fluids fall below normal
- During summer, due to excessive sweating, more water is lost, the body fluids reduce. As a result, more and more water is reabsorbed by kidney tubules back into the blood and urine turns thick and yellow. To maintain water balance of the body, the following changes take place in the body.
- The glomerular filtration slows down due to decreased filtration pressure in the glomerular capillaries.
- The osmoreceptor cells of the hypothalamus send impulses to the posterior pituitary lobe to release ADH. ADH increases the reabsorption of water in the distal convoluted tubule and the collecting duct by making them more permeable to water.
- Less filtration and more reabsorption of water leads to the discharge of small amounts of hypertonic urine. This raises the volume of body fluids to normal.
Urine is slightly thicker in summer than in winter
- During summer, when the temperature is high, lot of water is lost from the body through sweating (perspiration). To make up for this loss, more and more water is reabsorbed by the kidney tubules and put back into the blood making urine more concentrated (thicker).
Why do we feel thirsty despite drinking water at regular intervals?
- If enough quantity of ADH is not released, water cannot be retained by the kidney tubule and is lost as urine. This causes increase in thirst. Whatever water we drink is lost again. In severe conditions, it causes dehydration and electrolyte imbalance in the body.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Renal Failure And Artificial Kidney
- Artificial kidney is used to filter the blood of a patient whose kidneys are damaged. The patient is said to be put on dialysis and the process of purifying blood by an artificial kidney is called haemodialysis.
- Artificial kidney is a dialysis machine that contains a number of tubes, suspended in dialysing fluid. The patient’s blood is passed through these tubes. During this process, nitrogenous waste products from the blood pass into dialysing fluid. The purified blood is pumped back into the patient’s body.
UP Board Notes for Class 10 Science Chapter 9 Excretion-Elimination Of Body Wastes Summary
- The removal of waste products formed in the body due to metabolic activities is termed excretion.
- Kidneys in human beings are said to be retroperitoneal because they lie behind the peritoneal lining of the abdominal cavity.
- Each kidney In longitudinal section shows two distinct regions an outer renal cortex and an inner renal medulla.
- Nephron is the functional unit of kidney.
- Each nephron consists of a Malpighian capsule, anephric tubule and a collecting tubule.
- Urine formation involves three main processes ultrafiltration, tubular reabsorption and tubular secretion.
- Yellow colour of the urine is due to the presence of a pigment, urochrome, derived from the breakdown of haemoglobin of worn-out RBCs.
- The water and osmotic concentration of blood is maintained by the kidney. This phenomenon is known as osmoregulation.
- The process of purifying blood by the use of an artificial kidney is called dialysis.
