UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Learning Objectives
After completing this chapter, you will be able to:
- Describe the composition, physical characteristics and functions of blood; describe the ABO blood groups and the Rh factor;
- Describe the structure and functions of the heart;
- Trace the pathway of blood circulation through the heart;
- Name the major blood vessels entering and leaving the heart;
- Describe the cardiac cycle and heart sounds;
- Differentiate between arteries, veins and capillaries;
- Differentiate between systemic and pulmonary circulations;
- Describe the structure and distribution of lymphatic vessels and their functions;
- Differentiate between blood and lymph.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Circulation Of Fluids In Humans
- In human beings, a rapid supply of nutrients, oxygen and hormones to various tissues and the immediate disposal of waste products are essential requirements. So, our body has a specialized circulatory system. The circulatory system has three main parts.
- Circulatory medium – Blood, tissue fluid and lymph
- Blood vessels – Arteries, veins and capillaries
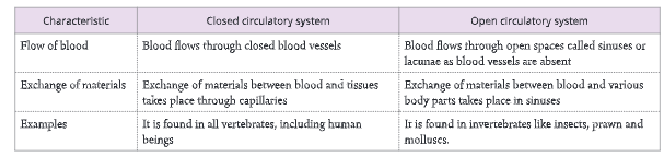
- Pumping organ – Heart The circulatory system, in different animals, are of two types – open and closed. The differences between the two are given in Table.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Circulatory Medium – Blood, Tissue Fluid and Lymph
Our body has three different types of fluids:
- Blood- Found in the heart and blood vessels (arteries, veins and capillaries)
- Tissue fluid – Found in the intercellular spaces
- Lymph-Found in the lymph vessels and lymphatic organs (e.g. spleen and tonsils)
| Class 10 Science | Class 11 Chemistry |
| Class 11 Chemistry | Transformation of Sentences |
| Class 8 Maths | Class 8 Science |
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Blood – Composition And Functions
- An average human being has about 5.5 litres of blood in his body. About 50-60 per cent of the blood is a fluid called plasma and the remaining 40-50 per cent is made of cellular elements called corpuscles that are held in suspension. Blood always flows from the heart through the arteries and back to the heart through the veins.
Physical properties of the blood
- Blood is a red-coloured, viscous and complex tissue fluid. It is salty in taste and slightly alkaline with a pH range of 7.35-7.45. Blood constitutes about 6 to 8 per cent of the total body weight.
Composition of blood
- Blood is made up of two main components – plasma (fluid part) and cellular or formed elements (blood corpuscles, solid part).
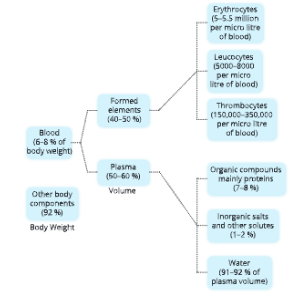
Plasma – the fluid part
- Plasma is a straw-coloured aqueous part of the blood in which formed elements remain suspended. It forms about 50-60 per cent of the blood volume. Plasma contains water (about 90-92 per cent), inorganic salts (about 1-2 per cent) and organic compounds (about 7-8 per cent).
- Plasma = Blood – Formed elements
- Plasma from which the protein fibrinogen has been removed is called serum.
- Serum Plasma – Fibrinogen
Cellular elements
- In human beings, three types of cellular elements are found suspended in the plasma.
- Red blood corpuscles (RBCs) or erythrocytes
- White blood corpuscles (WBCs) or leucocytes
- Platelets or thrombocytes
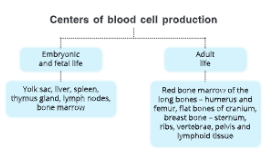
The process by which new blood cells are formed is called haemopoiesis or haematopoiesis.

UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Red Blood Corpuscles (RBCs)
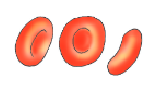
- Red blood corpuscles or erythrocytes (Gk. erythrose: red) are biconcave and enucleated (i.e. without a nucleus), disc-like cells which are flat in the centre, and thick and rounded at the periphery. Young RBCs have a nucleus, but as they mature, the nucleus degenerates. Such a shape is of great advantage to RBCs as it increases their surface area.
- Due to the lack of organelles (such as mitochondria and endoplasmic reticulum), their oxygen demand is negligible.
- The RBCs are very small in size. This small size helps them in absorbing oxygen and enables them to move in very fine blood capillaries throughout the body of a person.
- RBCs are produced in the bone marrow of long bones, ribs, vertebrae and skull bones. The average life span of erythrocytes is about 120 days.
- Their average number ranges from 5 million to 5.5 million in human males and 4.5 million to 5 million in human females.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Haemoglobin (Hb)
- The RBCs have a colourless spongy body which contains haemoglobin. The haemoglobin is the respiratory pigment which is composed of an iron-containing part known as haeme and a protein part known as globin.
The oxygen after diffusing into blood capillaries combines with the iron-containing part of RBCs and forms oxyhaemoglobin. - Absence of a nucleus and other organelles makes RBCs more efficient
1. RBCs in mammals are enucleated when mature, that is, they lack a cell nucleus. This is attributed to their oxygen-carrying capacity. These cells become more efficient in their work because of the following reasons:
- More space is available for haemoglobin which carries oxygen.
- The shape changes to a biconcave disc rather than a normal sphere, increasing the surface area volume ratio for a better exchange of oxygen and carbon dioxide.
- The biconcave shape optimises the flow of the blood within blood vessels as these cells move in a laminar flow, i.e. in parallel rows without any swirls.
- No nucleus means no DNA, so proteins cannot be synthesized. Their inability to carry out protein synthesis means they cannot be attacked by many viruses.
2. RBCs in mammals do not have mitochondria which is the site of cellular respiration. This ensures that all of the oxygen taken up by these cells from the lungs is delivered to the target tissue and not utilised by the cell itself.
3. RBCs also lack organelles like the Golgi apparatus and endoplasmic reticulum. This decreases their size markedly from 24 u to 7-9 μ and makes them small enough to pass through the smallest capillaries.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System White Blood Corpuscles (WBCs)

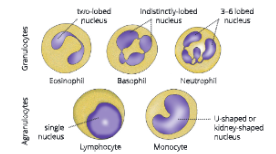
White blood corpuscles
- White blood corpuscles or leucocytes (Gk. Leucos: white) are rounded or Fig. irregular-shaped cells. They are capable of amoeboid movement. They are colourless since they lack haemoglobin.
- They are produced in the bone marrow. Leucocytes are of two types –
- granulocytes (contain granules in their cytoplasm and have lobed nuclei) and
- agranulocytes (lack granules in their cytoplasm and have unlobed nuclei).
1. Granulocytes
Granulocytes are spherical in shape and larger than the red blood cells. They have lobed nuclei and their cytoplasm contains granules. There are three types of granulocytes – (a) neutrophils, (b) basophils and (c) eosinophils.
- Neutrophils: Neutrophils account for 50-70% of the WBCs in our blood. Their cytoplasm contains very fine granules. The nucleus has 3-6 lobes. The granules stain with both acidic and basic. Dyes. Neutrophils are highly phagocytic in nature. Neutrophils contain special proteins called defensins, which have an antimicrobial activity against germs.
- Basophils: Basophils account for only 0.5% of the total WBCs. They are of the same size or slightly smaller than neutrophils. The nucleus is indistinctly lobed. The cytoplasmic granules stain with basic dyes. Basophils produce histamine and heparin, which intensify the inflammatory response in an allergic reaction. During inflammation, the blood vessels dilate making their walls leaky for leucocytes to squeeze out of the blood capillaries and engulf the germs. This process is known as diapedesis.

- Eosinophils: Eosinophils account for 1-4% of the total WBCs. The nucleus is two-lobed. The cytoplasmic granules are large and rough and stain dark red with acidic dyes (e.g. eosin). They phagocytose the antigen-antibody complex. They release chemicals to combat inflammation during an allergy.
2. Agranulocytes
Agranulocytes’ nucleus is single and typically spherical or kidney-shaped. The cytoplasm does not contain granules. There are two types of agranulocytes – (a) lymphocytes and (b) monocytes.
- Lymphocytes: Lymphocytes account for about 25% of the total WBCs. The nucleus is large, and spherical, with a dent-like depression on one side, which occupies most of the cell volume. They produce antibodies and play a crucial role in immunity.
- Monocytes: Monocytes are the largest leucocytes and account for 3-8% of the total WBCs. The nucleus is large and U- or kidney-shaped. They arephagocytic in nature and ingest germs and clean up damaged cells. Hence, monocytes are referred to as wandering macrophages.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Functions Of WBCs
- WBCs help in destroying solid substances and germs, especially bacteria, by engulfing them. This defensive process of fighting against disease-causing germs is termed as phagocytosis. Neutrophils are most active in this role. By doing so they protect the body from diseases, i.e. they are responsible for
immunity.
- They also help in the formation of antibodies which neutralize or kill the germs that enter our body.
Inflammation
- It is a defensive response of the body to tissue damage by microbes, physical agents or chemical agents. It is characterised by four fundamental symptoms – redness, pain, heat and swelling.
- The following reasons of inflammation are given below:
- Vasodilation, i.e. increase in diameter of surrounding blood vessels.
- Increased permeability of blood vessels. It allows defensive substances in blood to enter the injured area and phagocytosis occurs.
Thus, it is to be clearly understood here that inflammation is not a role of WBCs but phagocytosis at the point of inflammation is carried out by neutrophils and monocytes. In case of an allergic reaction, basophils intensify the inflammatory response.
Pyogenesis
- (pyo = pus; genesis = to produce)
- The phenomenon of pus production during an inflammation is pyogenesis. Pus is a thick whitish fluid which contains living and dead WBCs and dead tissue debris.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Blood Platelets (Thrombocytes)
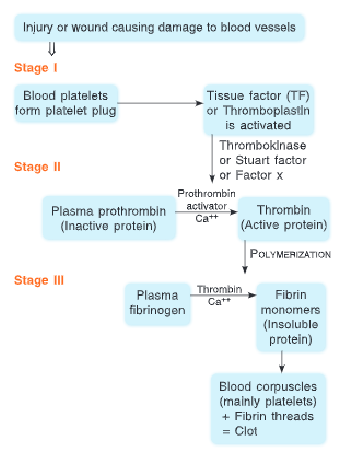
- Blood platelets are colourless, oval or round (plate-like in active form), cytoplasmic fragments formed from giant cells of the bone marrow. These are found floating in the blood. These are enucleated (without a nucleus), bound by a membrane and contain a few organelles. Their life span is about 5-10 days. Thrombocytes help in blood clotting. They release a chemical, thromboplastin that initiates the process of clotting of blood. They can repair slightly damaged blood vessels.

Let us understand…
- An antigen is a protein produced by the body in response to the presence of an antigen and combines specifically to that antigen. WBCS act as antibodies by phagocytosing the antigen.
- Toxin is a poisonous substance produced by an antigen (foreign body) which has unfavourable effects on the body of the organism. In other words, a toxin is toxic the Infected organism.
- Toxoid is an activated or weakened toxin produced by an antigen which is not toxic anymore. However, it is still capable of acting as an antigen and hence, is used as a vaccine which stimulates production of specific antibodies in the blood of an organism.
- Antibody neutralizes a specific antigen.
Blood diseases
- An increase in the number of RBCs much more than normal is called polycythemia.
- A decrease in the RBC count is called erythrocytopenia.
- An enormous increase in WBCs at the cost of RBCs causes leukaemia – the blood cancer.
- A decrease in the WBC count is known as leucopenia.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Functions Of Blood
Blood is a complex fluid which performs a number of roles in our body. It transports, regulates and protects.
1. Transportation
- Transport of nutrients: The digested food substances are absorbed by the blood at the site of absorption (small intestine) and transported to different organs of the body.
- Transport of respiratory gases: Blood transports oxygen from the lungs to the tissues and carbon dioxide from the tissues back to the respiratory surface, i.e. lungs.
- Transport of waste products: The metabolic waste substances produced in the body are transported by the blood to the excretory organs.
- Transport of body secretions: Blood transports chemical secretions like hormones, from the site of their secretion (endocrine glands) to the target organs.
2. Regulation
- Regulation of body temperature: Blood helps to control the body temperature by evenly distributing the heat produced in one part of the body to different parts.
- Maintenance of pH: The plasma proteins are amphoteric in nature, i.e. they act as a buffer and thus maintain the pH of blood.
- Water balance: Blood maintains water balance to a constant level by bringing about constant exchange of water between the circulating blood and the tissue fluid.
3. Protection
- Clotting of blood protects against blood loss: Prothrombin and fibrinogen proteins of plasma help in blood clotting at the site of injury. This prevents blood loss.
- Defence against infection: Blood contains WBCs that are phagocytic in nature. WBCs also produce antibodies that destroy the bacteria, after neutralizing their toxins, and thus, play a protective role.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Clotting Of Blood
- Blood is in a fluid state when inside the blood vessels. Blood does not clot in uninjured vessels due to the presence of natural anticoagulants called heparin and antithrombin, produced in the liver. Blood usually clots after it escapes from the blood vessels.
- When blood vessels get damaged due to any external injury or an internal cause, three basic mechanisms become operational in the following sequence:
Step 1. Vascular spasm occurs. When a blood vessel (artery or vein) other than a capillary is injured, the smooth muscles in its wall contract to reduce blood loss.
Step 2. Platelet plug formation occurs. The platelets get activated on coming in contact with the damaged blood vessel. Platelets undergo drastic changes in their shape and release several substances involved in the step of blood coagulation. The activated platelets become sticky and form a platelet plug at the damaged spot. This plug is initially loose and is tightened by the fibrin threads formed in the next step.
Step 3. Coagulation of blood occurs. The process of clotting of blood is known as coagulation. A clot is a network of insoluble protein fibres called fibrin in which the cellular components of the blood get trapped. Coagulation is a complex process in which several coagulation factors (I to XIII) come into action in a definite sequence. It can be divided into three basic stages as follows:
Stage 1. Formation of prothrombin activator: A protein called Tissue Factor (TF) or thromboplastin found on the surface of various body cells such as brain, lungs and intestines initiates the formation of prothrombin activator. It is a cascade of events which ends with the activation of the enzyme thrombokinase also called factor X or Stuart factor which in the presence of Ca++ ions forms a prothrombin activator. The Stuart factor is not released by platelet disintegration. However, bursting of platelets provides phospholipids that activate this factor.
Stage 2. Conversion of prothrombin to thrombin: The prothrombin activator formed in stage 1 now converts prothrombin to thrombin with the help of Ca++ ions.
Stage 3. Conversion of fibrinogen to fibrin: Fibrinogen is a soluble protein found in the plasma. Thrombin formed in stage 2 now converts soluble fibrinogen to insoluble fibrin in the presence of Catt ions.
The platelet plug is strengthened by fibrin which forms a network at the site of the injury. Thrombin also causes more platelets to adhere to each other thus strengthening the clot.
Clot Vs Thrombus
- Intravascular clot formed in an unbroken blood vessel is called a thrombus. Every clot is not a thrombus.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Blood Groups And Blood Transfusion
Blood groups
- In 1901, Karl Landsteiner, a German biochemist, proposed that the blood of different individuals has some biochemical differences. There are two types of proteins in the human blood.
- Agglutinogen or antigen is present on the surface of RBCs. It is called the corpuscle factor.
- Agglutinin or antibody is a protein present in the blood plasma and is called the plasma factor. There are two kinds of antigens, A and B, and two kinds of antibodies, a and b, in the blood. Antigen A and antibody a are antagonistic or incompatible and cause self-clumping. Similarly, antigen B and antibody b are incompatible and cause self-clumping. Antigen A is compatible with antibody b and antigen B is compatible with antibody a.
- On the basis of the type of antigen present on the surface of RBCs as given below, a system of blood groups known as ABO system, in which there are four blood groups, is recognized in the human blood.
- Group A with antigen A and antibody b.
- Group B with antigen B and antibody a.
- Group AB with both A and B antigens but no antibodies.
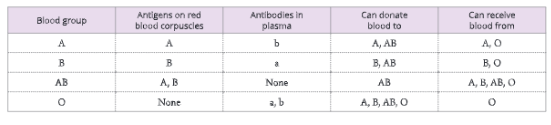
- Group O has no antigen but both antibodies a and b.
Blood transfusion
- Blood transfusion is a procedure of transfer of blood or blood components from one person (donor) into the bloodstream of another person (recipient). The antigens of the donor’s blood can react with antibodies of the recipient’s blood and cause clumping of RBCs. Thus, antigen A present in the RBCs of blood group A individuals reacts with antibodies of plasma of blood group B individuals and vice versa. This phenomenon is known as agglutination. Agglutination may cause serious consequences and even prove fatal.
- The RBCs of blood group O individuals lack antigens and are not clumped by antibodies present in the serum of the recipient’s blood. It means blood group O can be given to persons with blood group O, A, B or AB. Hence, persons with blood group O are called universal donors.
- However, persons with blood group AB lack antibodies in their plasma, so they can receive blood from A, B, O or AB blood groups. Such persons are called universal recipients.
Rh factor (Rhesus antigens)
- Landsteiner and Wiener discovered in 1940 that the surface of human RBCs contains a protein that is also found in the RBCs of Rhesus monkeys. So, it was termed an Rh antigen or Rh factor. Those persons who have this factor are called Rh-positive and others as Rh-negative.
- Both Rh-positive and Rh-negative persons are quite normal. The problem arises when Rh- blood comes in contact with Rh+ blood either due to blood transfusion or during pregnancy.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Incompatibility During Blood Transfusion
- The Rh-blood can be given safely to an Rh+ individual. When Rh* blood is transfused into an Rh- person, the recipient forms antibodies in her/his blood. However, no complications develop after the first transfusion.
- In case of a second transfusion of Rh* blood to an Rh person, the recipient’s anti-Rh factors attack and destroy the donor’s red blood corpuscles. Therefore, it is always advised that the patient’s Rh factor is determined before transfusion.
Incompatibility during pregnancy
- A serious problem arises if an Rh™ mother is carrying an Rh foetus. The Rh blood of the foetus will stimulate the formation of anti-Rh factors or antibodies in the mother’s blood. During the first pregnancy, enough antibodies are not produced to harm the foetus.
- During the second pregnancy, if the foetus is Rh*, more antibodies will be produced in mother’s blood. Due to the cumulative effect of antibodies produced the second time, in addition to the antibodies already present in mother’s blood, a large number of RBCs of the foetus are destroyed. This causes death of the foetus. This called erythroblastosis fetalis.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Parts Of Human Circulatory System
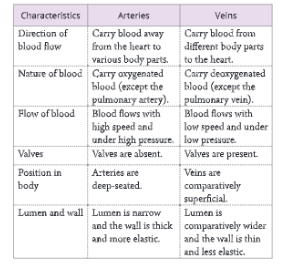
Blood vessels 1
- The blood vessels are a system of channels through which the blood flows. There are three kinds of blood vessels – arteries, veins and capillaries.
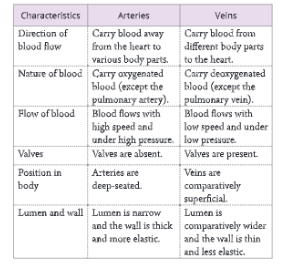
1. Arteries are the blood vessels that carry blood away from the heart to the various parts of the body.
- All arteries (except the pulmonary artery) carry oxygenated blood.
- An artery has thick and elastic muscular walls.
- Arteries have a small lumen without valves.
- The blood flows in spurts in arteries corresponding with contractions of the ventricles in the heart.
2. Capillaries are microscopic, thin vessels that carry blood from arterioles to small their venules.
- They are found abundant in those tissues or organs where the rate of metabolism is very fast.
- Capillaries are made of single-layered endothelial tissue with a very narrow lumen.

- Their wall is very thin, having a tunica intima Capillaries connect arteries and veins.
- Their wall is very thin, having a tunica intima(also called tunica interna) layer only. They have a large lumen with valves.
Their walls are thin to facilitate the exchange of food material, gases and waste between the blood and the tissues.
Functions of capillaries
- To allow inward and outward diffusion of glucose, amino acids, urea, etc.
- To allow diffusion of oxygen into intercellular fluids and inward diffusion of carbon dioxide from intercellular fluids.
- To allow movement of leucocytes through capillary walls. (RBCs and proteins do not move out of the capillary walls)
- Diagrammatic relationship between arteries, veins and capillaries
3. Veins are the blood vessels that carry blood from the body parts to the heart.
- All veins (except the pulmonary vein) carry deoxygenated blood.
- The wall of a vein is thinner as compared to the arterial wall.
- They have a wider lumen.
- Blood flows uniformly within veins.
- Veins have semilunar valves that prevent the backward flow of blood. These valves are formed from folds of the inner walls of the veins. Forward pressure of the blood forces the valve to open and the blood flows towards the heart, whereas the backflow of the blood causes the valve to close.
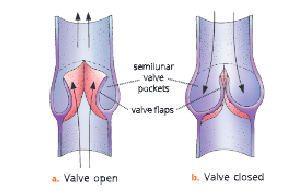
- Action of a semilunar valve in a vein
- Differences between an artery and a vein are given have the power to constrict or dilate as their wall lacks in Table.
Vasodilation and Vasoconstriction
- The smooth muscle layer of arteries and veins (called the tunica media) has a nervous supply with it. When these nerves are stimulated, the smooth muscles contract, and squeeze
- the wall of the vessel leading to a narrow lumen. Such a decrease in the lumen size is called vasoconstriction.
- When the stimulation is removed, the muscle fibres relax and the lumen size increases leading to vasodilation.
- This clearly indicates the role played by the smooth muscle fibres in the walls of arteries and veins in these
phenomena. It is to note here, that capillaries do not muscle fibre layer. - When we walk in the hot sun, our face turns pink due to vasodilation of the blood vessels supplying blood to the skin capillaries. There is an increase in the flow of blood into the capillaries on the surface of the skin. On the contrary, the skin turns pale due to vasoconstriction when it is too cold.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart
Position, shape and size of the heart
- The human heart is located between the lungs in the thoracic cavity, with its lower end inclined towards the left. The heart is a hollow, fibromuscular organ and is somewhat conical in shape. It is about the size of one’s fist. It’s pointed end projects to the left.
- The heart is enclosed by a double-layered membranous sac called the pericardium. It protects the heart from mechanical injury. The space between two pericardial membranes is the pericardial space, which is filled with the pericardial fluid. The pericardial fluid keeps the heart moist and reduces friction between the heart wall membranes. The human heart is made of cardíac muscles or myocardia which contract rhythmically by self-generated impulses.
External structure of the heart
- The human heart is a four-chambered organ divided by septa into two halves – the right half and the left half. Each half consists of two chambers – the upper, small-sized auricle or atrium and a lower, large-sized ventricle.
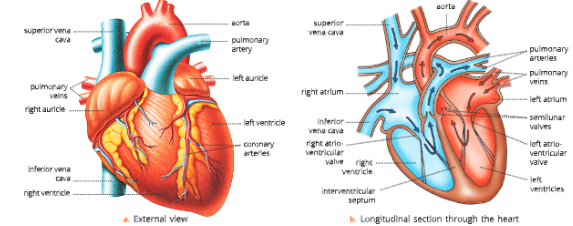
Internal structure of the heart
- Internally, the heart has the following main components – four chambers (two auricles and two ventricles), great blood vessels that carry blood to the heart and away from it, and various apertures and valves.
Chambers of the heart
- Auricles – The receiving chambers: The auricles or atria are thin-walled chambers and are separated from each other by an inter-auricular septum.
- Ventricles – The discharging chambers: The ventricles are thick-walled chambers and are separated from each other by an obliquely placed inter-ventricular septum. The wall of the left ventricle is the thickest because it has to pump blood into vessels, which in turn carry the blood to long distances up to the head, trunk and extremities. The right ventricle pumps blood to the pulmonary arteries, which carry it to the lungs. The walls of the atria are thinner than that of ventricles because they just have to deliver blood into the ventricles.
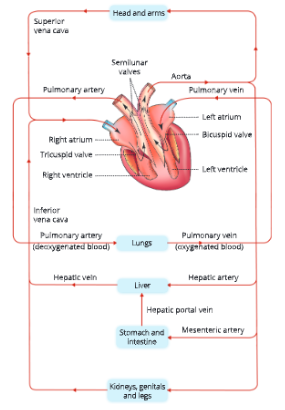
Great blood vessels of the heart
the blood vessels that enter or leave the heart are called great blood vessels.
Blood vessels entering the heart
1. The right auricle receives blood from three blood vessels.
- Superior (Anterior) vena cava or Perceval brings deoxygenated blood from the head and upper region of the body.
- Inferior (Posterior) vena cava or postcaval brings deoxygenated blood from the lower region of the body.
- Coronary sinus brings deoxygenated blood from the heart’s wall itself into the right auricle.
2. The left auricle receives four blood vessels.
- Pulmonary veins – The left auricle receives blood from two pairs of pulmonary veins, one pair from each lung. These bring oxygenated blood from the lungs.
Blood vessels leaving the heart
- Pulmonary artery arises from the right ventricleand carries deoxygenated blood to the lungs for oxygenation.
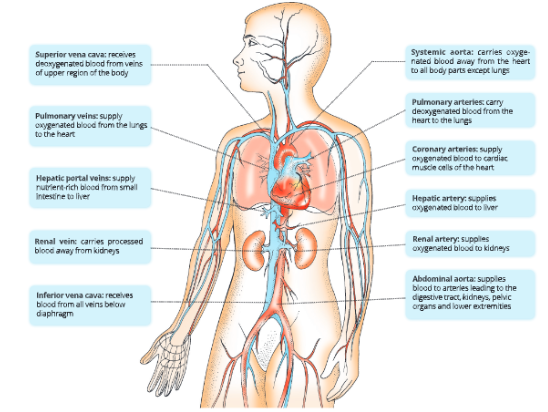
- Systemic aorta originates from the left ventricle and supplies oxygenated blood to all body parts, except the lungs.
- Coronary arteries arise from the base of the aorta. These supply blood to the heart muscles. If coronary arteries get blocked, then it can cause heart attack.
shows the location and functions of major blood vessels of human cardiovascular system.
Apertures and valves in the heart
- There are four valves in the heart which control the flow of blood within the heart and its passage to various parts of the body through the great blood vessels.
- The bicuspid valve (also called the mitral valve or left auriculo-ventricular valve) guards the opening of the left auricle into the left ventricle. This valve consists of two flaps or cusps.
- The tricuspid valve (also called the right auriculo- ventricular valve) guards the opening of the right auricle into the right ventricle.
Both, the bicuspid and the tricuspid valves allow blood to pass from auricles to the ventricles and prevent the backflow of blood. - Semilunar or pulmonary valves are present at the base of the pulmonary artery. These valves allow the flow of blood from the right ventricle to the pulmonary artery and check the backflow of blood into the ventricles.
- Aortic semilunar valve is present at the point of origin of the aorta. In all, there are three semilunar valves in the vessels. They allow blood to pass from left ventricle to the aorta and check the return of blood into the ventricles.
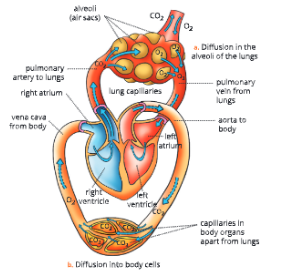
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System Double Circulation
- The circulation of blood in the human heart is called double circulation because the blood enters and leaves the heart twice in each heartbeat. Circulation of blood between the heart and body organs (except lungs) is called systemic circulation. Circulation of blood between the heart and the lungs is called pulmonary circulation.
Systemic circulation
- The left ventricle pumps the oxygenated blood into the systemic aorta. Aorta gives off branches to all the organs of the body except lungs.
- From these arteries, oxygen is diffused into the tissues. Deoxygenated blood from visceral organs is brought to the right auricle by superior and inferior venae cavae. This part of circulation from the left ventricle to the right auricle of the heart via body tissues (except lungs) is called systemic circulation.
Pulmonary circulation
- The circulation of blood from the right ventricle to the left auricle of the heart via lungs is called pulmonary circulation. The right ventricle pumps deoxygenated blood to the lungs for oxygenation. Oxygenated blood from the lungs is returned to the left auricle by four pulmonary veins.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart Cardiac Cycle – Systole and Diastole
- The sequence of events, that take place during the completion of one heartbeat, is known as the cardiac cycle. It involves repeated contraction and relaxation of the heart muscles. A contraction is termed as systole and a relaxation is termed as diastole.
- One complete heartbeat or cardiac cycle consists of systole and diastole both atria and both ventricles followed by a short pause. It lasts for about 0.8 seconds.
- The events that take place during the completion of one heartbeat are -the auricular systole, the ventricular systole and the joint diastole or complete cardiac diastole.
1. Auricular systole: The two auricles act as a pump to force the venous blood into the ventricles. The ventricles are in diastole at this time. During auricular systole, the auricular muscles contract. and the openings of venae cavae and pulmonary vein close. The tricuspid valve and bicuspid valve
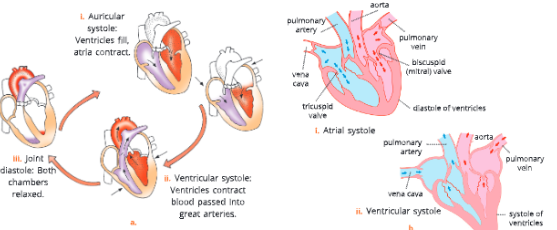
- open and the blood enters the ventricles through these valves. At the end of an atrial systole, as the two auricles relax, more venous blood is passed from the great veins into the atria to fill them up.
2. Ventricular systole: With the onset of atrial diastole the ventricles start contracting. The bicuspid and tricuspid valves (also known as atrioventricular or AV valves) close to prevent the backward flow of blood from ventricles to the atria. When the pressure in the ventricles increases, semilunar valves open and blood is passed into the great arteries.
3. Joint diastole: At the end of a ventricular systole, the ventricles relax. Also at this stage, the atria are still in their diastole. Since all the heart chambers are in diastole, this stage is called joint diastole. During this phase, blood continues to flow into the auricles from the great veins. As the atria fill with blood, the pressure in them rises and becomes greater than that in the relaxed ventricles. Blood then flows from the auricles to respective ventricles through the AV valves.
How is cardiac cycle conducted?
- The heart is supplied by a network of nerves but these are not responsible for the initiation of the cardiac cycle.
- The heart can keep on contracting and relaxing without any stimulation from these nerves. However, the heart.
- has a regulating system of its own called the conduction system. It is a system of specialised muscle tissue which initiates and spreads the electrical impulses to stimulate a cardiac cycle.
It has the following parts:
- SA node or sinoatrial node: It is located in the wall of the right atrium near the opening of the superior vena cava. As it initiates each cardiac cycle and sets the pace or rhythm for the heart beat rate, it is called the pacemaker of the heart.
- AV node or atrioventricular node: It is located near the inferior part of the interauricular septum. The impulses initiated by the SA node make the atria contract and the electrical signals are received by the AV node.
- AV bundle or atrioventricular bundle: It is a tract of conducting fibres that arise from the AV node and run along the interventricular septum. The impulse travels through these fibres, also called the “Bundle of His”.
- Purkinje fibres: These fibres emerge from the Bundle of His as branches and spread into the myocardium of ventricles. These fibres stimulate the contraction of ventricles, hence called conduction myofibers.
Electrocardiogram (ECG)
- The muscle cells or fibres of the heart are specialised at certain parts of the heart to generate electric currents that cause a normal rhythmic heartbeat.
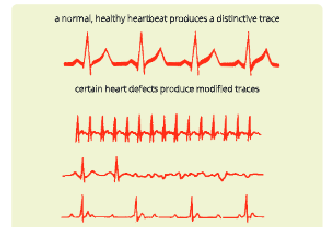
- A recording of the electrical events that control the cardiac cycle is called an electrocardiogram (ECG). The instrument used to record the changes is an electrocardiograph.
The ECG is a useful diagnostic tool for heart diseases like tachycardia (a high pulse rate above 100/minute), bradycardia (a slow pulse rate below 60/minute), ventricular fibrillation and heart block.
Pulse rate
- The rhythmic contraction of the heart can be felt as a jerk in certain arteries which are superficial in position. This is the arterial pulse. Each ventricular systole starts a new pulse. It proceeds as a wave of expansion throughout the arteries and disappears in the capillaries. The pulse rate is the same as the heartbeat rate. The pulse rate in a normal adult man is about 64-72 beats per minute while in a woman 72-80 beats per minute. The pulse rate in infants is about 140 beats per minute.
Heart sounds – Lubb and dubb
- The various valves present at the outlet and inlet of ventricles determine the direction of flow of blood in the heart. The opening and closing of these valves cause heart sounds. These sounds can be heard by using a stethoscope (an instrument that magnifies sounds and conducts them to the ear). These sounds are heard as ‘lubb’ and ‘dubb’ sounds.
- The lubb sound (first heart sound): This sound is caused by the vibrations initiated by the closure of tricuspid and bicuspid valves accompanied by the contraction of ventricular muscles at the start of ventricular systole. It is also called a systolic sound. Lubb sound is low-pitched, not very loud and is of a long duration.
- The dubb sound (second heart sound): This sound is caused by the closure of the semilunar valves and marks the end of ventricular systole and beginning of ventricular diastole. The dubb sound is high-pitched, louder and shorter in duration.
An abnormal heart sound is called a murmur. This is caused problems with the valves.
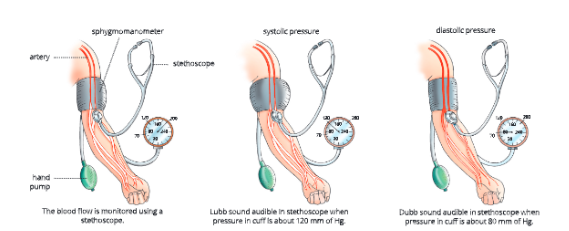
Blood pressure
- It is the force with which blood pushes against the walls of the arteries. It is generally measured in terms of how high it can push a column of mercury. When the ventricles contract, the pressure of blood inside the arteries is highest and this pressure is termed as systolic blood pressure.
- In a healthy young human being, it is about 120 millimetres of mercury (120 mm Hg). When ventricles relax, the pressure of blood inside the arteries is comparatively less and this pressure is termed as diastolic pressure. It is about 80 millimetres of mercury (80 mm Hg) in a healthy young man. Thus, a healthy young man is said to have a normal blood pressure of 120/80 mm of Hg. The instrument used to measure blood pressure is called a sphygmomanometer.
- Blood pressure =systolic/diastolic = 120/80mm of Hg
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart Portal System
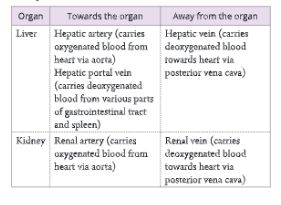
- A vein that does not carry deoxygenated blood directly to the heart but forms a network of capillaries on another organ before reaching the heart is called a portal vein. It begins and ends in capillaries. The components of the portal vein constitute the portal system. In human beings, two main portal systems – the hepatic and the hypophyseal portal systems are present.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart Hepatic Portal System
- The venous blood from gastrointestinal organs and spleen is drained into the liver before returning to the heart. Veins from various regions of the gastrointestinal tract and spleen unite to form the hepatic portal vein. It divides into two branches, right and left, which enter into the corresponding liver lobes and break up into capillaries to supply blood. A pair of hepatic veins carry this deoxygenated blood from the liver to the inferior vena cava.
Why is there a need for the hepatic portal system?
- The blood in hepatic portal vein is rich in nutrients absorbed from the digestive tract. The liver absorbs substances like glucose and stores it as glycogen for use when required. It also modifies other substances so that they can be used by cells. It detoxifies harmful substances in the blood. It also destroys bacteria by phagocytosis.
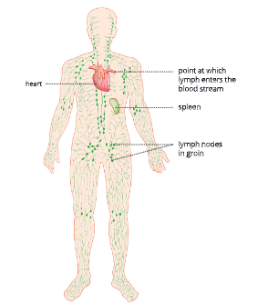
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart Lymphatic System
- The lymphatic system comprises a colourless fluid called lymph and a network of fine channels namely, lymphatic capillaries (lacteals) and vessels (ducts), and the lymph nodes.
Lymph
- Lymph is a colourless fluid. It is a part of the tissue fluid which in turn is a part of blood plasma. So, the composition of tissue fluid and lymph is the same as that of blood plasma but tissue fluid and lymph have lower protein contents.
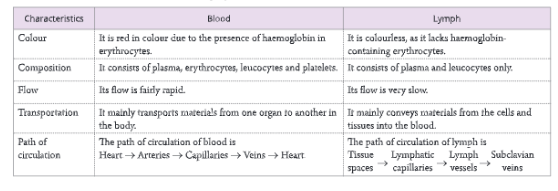
- Lymph consists of a fluid matrix in which the white blood corpuscles or leucocytes are present. Unlike blood, lymph does not have red blood corpuscles, platelets and plasma proteins.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart The Circulatory System Functions of The Lymph
The lymph performs many functions.
- It carries carbon dioxide and nitrogenous waste materials that diffuse into the blood through the tissue fluid.
- It carries lymphocytes and antibodies from the lymph nodes to the blood.
- It transports fats (fatty acids and glycerol) from the intestine to the blood.
- It destroys microorganisms and foreign particles in the lymph nodes.
- It drains excess tissue fluid from the intercellular spaces back into the blood.
- It carries the plasma protein macromolecules, synthesized in the and horn endocrine glands to the blood.
Lymph vessels or lymphatics
- The lymph capillaries join to form the lymphatic vessels. These lymph vessels are like capillaries but have comparatively thin walls and numerous valves. The smaller lymphatic vessels unite to form larger vessels and they unite to form two main lymphatic ducts.
- The lymph vessels at the right side of the head, neck and the right arm enter into a large vessel, the right lymphatic duct which opens into the right subclavian vein.
Lymph nodes
- At specific points in the lymph vessels, there are enlargements like beads of a string. These are called lymph nodes. Lymph nodes contain lymphocytes, plasma cells and macrophages. The lymph is filtered through the lymph nodes. The macrophages remove microorganisms and foreign particles from the lymph. The lymphatic nodes also add lymphocytes and antibodies to the lymph from where these are carried to the blood.
- Lymph nodes are abundant in the regions of neck, armpit and groin.
- Tonsils and adenoids are masses of lymphatic tissues.
The thymus and spleen are important lymphatic organs of the body.
Tonsils
- Tonsils are aggregations of lymphatic nodules enclosed by brane. These are located in a ring at the junction of oral cavity and pharynx.
Functions of tonsils
- Their location is best suited to protect the body against entry of any foreign substance through the oral cavity.
- They also produce lymphocytes and antibodies.
Spleen
- Spleen is the largest mass of lymphatic tissue found in our body. It measures about 12 cm in length and is located in the region between the fundus of stomach and diaphragm. It is covered by the peritoneal membrane.The tissue of spleen is of two types:
- White pulp – The lymphatic tissue
- Red pulp – Sinuses filled with venous blood and tissue cords consisting of macrophages, lymphocytes and granulocytes.
Functions of spleen
- It produces antibodies, phagocytic cells and destroys dead RBCs and platelets.
- In embryonic stage, it produces RBCs.
- It also acts as a reservoir of blood which is released during emergencies such as haemorrhage.
UP Board Notes For Class 10 Science Chapter 8 The Circulatory System The Human Heart Summary
- The flow of extracellular fluid in the body is called circulation and the organs concerned with this transport form the circulatory system.
- Human beings have an efficient circulatory system. It consists of:
- A circulatory medium – blood
- A system of blood vessels – arteries, veins and capillaries
- A pumping organ heart.
- Blood is made up of plasma and cellular elements. The cellular elements include RBCs, WBCs and platelets.
- Blood does not clot in uninjured vessels due to the presence of a strong, natural anticoagulant called heparin or antithrombin, produced by the liver.
- The glycoprotein or corpuscle factor present on the surface of RBCs and a protein or the plasma factor present in the blood plasma determine the type of blood group of a person. Blood groups in humans are of four types (A, B, AB, O) in ABO grouping system.
- Blood of group O can be given to any blood group, hence people with blood group O are called universal donors.
- Persons with blood group AB can receive blood from all blood groups, hence, are called universal recipients.
- All arteries carry oxygenated blood, except pulmonary arteries, which carry deoxygenated blood from the heart to the lungs for oxygenation.
- All veins carry deoxygenated blood except pulmonary veins, which carry oxygenated blood from the lungs to the heart.
- The human heart is a fibromuscular organ somewhat conical in shape. It is about the size of a fist. Its weight is about 300 g in an adult human being.
- The human heart is protected by a double-walled membranous sac called pericardium.
- The human heart is a four-chambered structure, divided by septa Into two halves the right and the left. Each half consists of an upper, small-sized, thin-walled chamber called auricle and a lower, large- sized and thick-walled ventricle.
- The left auriculo-ventricular aperture is guarded by the bicuspid valve, which consists of two flaps or cusps, and the right auriculo-ventricular aperture is guarded by the tricuspid valve made up of three flaps or cusps. These valves allow blood to pass from auricles to ventricles and also prevent the backward flow of the
blood. - Circulation of blood in the human heart is called double circulation because blood enters and leaves the heart twice. Circulation between the heart and the body organs except lungs is called systemic circulation. Circulation between the heart and the lungs is called pulmonary circulation.
- The sequence of events that take place during the completion of one heartbeat is known as cardiac cycle. It lasts for about 0.8 seconds.
- The rhythmic contraction of heart is felt as a jerk in certain arteries that are superficial in position. This is the arterial pulse. The pulse rate of a person is the same as the heartbeat rate.
- Blood pressure is the force with which blood pushes against the walls of arteries. The blood pressure of a healthy person is 120/80 mm Hg. The instrument used to measure blood pressure is called sphygmomanometer.
- The lymphatic system comprises of -lymph, lymphatic capillaries and vessels, and lymph nodes.
